Although overdenture is an age-old concept it has retained its popularity as a viable treatment option due its superior performance, while still being focused on a preventive approach. Preserving teeth on either side of the arch or placing bilateral implants will help enhance the retention and stability of a denture. Various attachments have been used over the preserved tooth or implant to aid in retention and stability. One of the most widely used attachments today is the stud attachment, but due to its cost patients, often do not opt for it. Therefore, this case report introduces a novel and alternative technique to fabricate the stud attachment without compromising its properties.
A completely edentulous patient goes through a
series of events following loss of teeth, like, loss
of function, esthetic, social and psychological
damage to the individual’s life, which may have
an enormous impact on self-esteem and health
of the patient1-2. Preservation of tooth or roots can
be an effective way to not only reduce bone loss,
but to also improve prosthetic outcome3-5.
An overdenture, which is a removable complete or partial denture resting on one or more remaining
natural teeth, root or/and implant, not only delays
the process of resorption but also preserves the
bone around retained roots and helps to improve
the masticatory efficiency.6
One of the reasons for the continued popularity of
tooth supported overdenture is the preservation of
proprioception which is provided by the periodontal
ligament of the tooth. The other advantage of
choosing an overdenture over a conventional
complete denture is, an increase in stability as
well as retention7.
To enhance the retention and stability of the
overdenture, various attachment systems can
also be used. An attachment is defined as “a
mechanical device for the fixation, retention, and
stabilization of a prosthesis, a retainer consisting
of a metal receptacle and a closely fitting part; the
former (the female matrix component) is usually
contained within the normal or expanded contours
of the crown of the abutment tooth and the latter
(the male patrix component), is attached to a
pontic or the denture framework”6. The various attachment systems available to connect the
implants to the overdenture are: Stud attachment,
Magnet attachments, Bar attachments, Telescopic
attachment, etc., stud and bar attachment being the
most widely used ones. The key advantages of stud
attachments are the feasibility of its use in V-shaped arches where a straight connection between the
tooth/implants cannot be established.8-9
An O-ring is an elastomeric retentive stud
attachment, shaped like the inner surface of a
tire and generally made up of silicone and nylon.
To aid in their longevity they have metal housings
that are incorporated within the denture base resin
either chair side or in the laboratory. The O-ring
assembly consists of ball head that is attached
to a post, with an undercut area or a retentive
groove. This assembly is usually fabricated from
precious or semi-precious alloys10. Some of the
advantages of an O-ring are - good retention,
ease of use, ease of maintenance, simplicity in
design, and ease of replacement11. Therefore, the
aim of this report was to fabricate an O-ring stud
attachment using implant prosthetic component.
A, 47-year-old male patient reported to our
department with a chief complaint of ill-fitting
maxillary dentures.
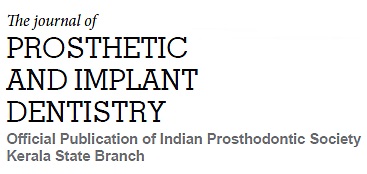
On examination, patient had existing maxillary
overdenture supported by copings on 13 and 23
[Fig.1].
Radiograph was advised to evaluate the condition
of the existing abutments. Since interarch space
was adequate and to enhance the stability of the
prosthesis, stud attachments were planned with
respect to 13 and 23.
Informed consent was obtained from the patient.
The post space was modified [Fig. 2], and
an indirect method was used for making the
impression of the post space using light body
polyvinyl siloxane impression material (Aquasil™
UltraLV, Dentsply, Caulk).
A pick-up impression was made using a custom
tray and a rubber-based impression material
[Fig.3] (Aquasil™ Ultra Monophase. DECA, Regular
Set-Dentsply, Germany).
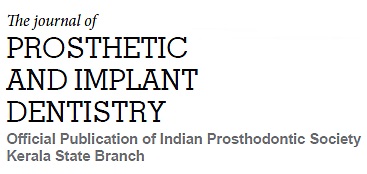
The impression was poured using Type IV Dental
Stone (Kalrock, Kalabhai Karson Pvt. Ltd., Mumbai,
India).
Border moulding and secondary impression of the
lower arch were carried out using the conventional
technique.
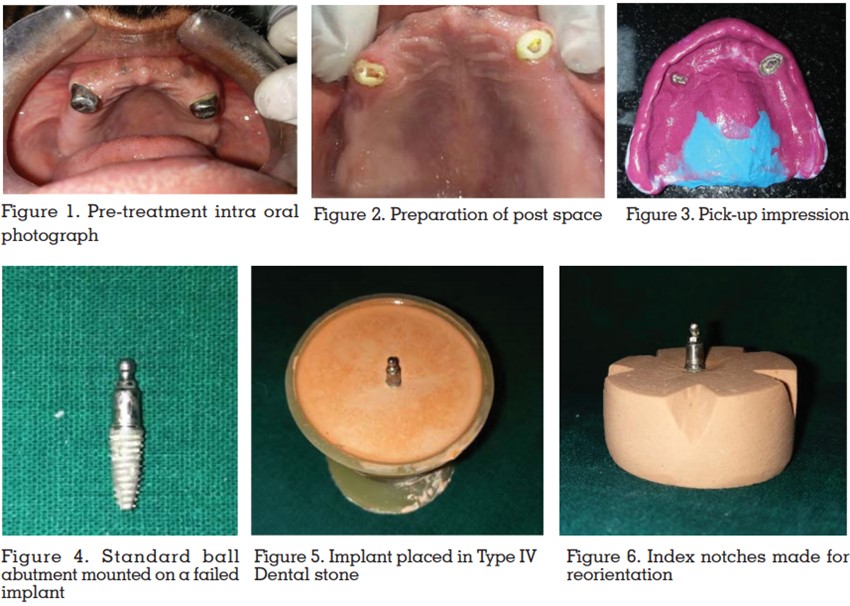
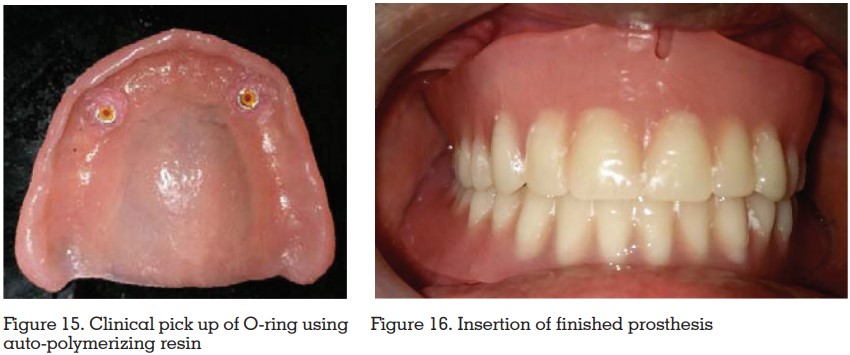
After the stud attachment was fabricated, they were
luted onto the abutment teeth using resin cement
(RelyX U200/3M ESPE-U200; Maxcem Elite/KerrMAX; Clearfil SA Cement/Kuraray-CSA).
A primary impression of the lower arch was made
with alginate and a special tray was fabricated on the primary cast after block out. Record rims were
made and the jaw relation was recorded. Teeth
arrangement was done and after a satisfactory
try-in, the denture was processed using heat cure
acrylic resin. After finishing and polishing of the
denture, vent holes were created in the maxillary
denture to create space for the O-ring. The O-ring
were picked up using auto-polymerizing resin [Fig.
15] while maintaining upper and lower dentures
in occlusion. Excess acrylic from the vent holes
was trimmed and the denture was finished and
polished and insertion was carried out [Fig.16].
Periodic follow-up was carried out.
It is well acknowledged fact that retaining natural
teeth, even with doubtful prognosis, or roots can reduce the rate of boneresorption12. Teeth showing
mobility can be retained and used as abutments
for overdentures. Preparation of abutment for
overdentures has the most dramatic effect on the
crown root ratio (CRR). It can alter the CRR from
1:1 to 1:2 or in some cases 1:3. Decreasing the
crown height shortens the length of the lever arm,
subsequently, exerting less lateral force onto the
attachments.
Which results in reduction of the horizontal
mobility shown by the abutment13. Various studies
have concluded that Abutment mobility can be
associated with periodontal health, as well as
to the improved biomechanical CRR. When the
teeth are preserved, the proprioception through
the periodontal ligament is also preserved, this provides the patient with better occlusal awareness,
good neuromuscular control and biting force14.
The physiologic advantages of overdentures are:
The other advantage of Overdenture is that can
easily converted to complete denture, in the event
of abutment failure, since they follow the principle
of complete denture construction12.
Rooney and Crum15 in their study with a 5 year
follow up established, through cephalometric
radiographs, an average loss of 0.6 mm of bone
height in the anterior part of the mandible in
overdenture patients when compared to a loss of
5.2 mm in complete denture patients.
Literatures states that the strategically selected
teeth in tactical positions can significantly enhance
the stability and retention of the overdenture
prosthesis16,17. Canines are most often retained, due
to their position at the corner of the dental arch and
also due to the shape, size and length of their root7.
Their relatively large root surface provides greater
periodontal and epithelial attachment, making
them the most important proprioceptive organ
in the oral cavity18. When the canines are absent
or lost, first premolars are used as alternative
because they are single rooted and because of
their favorable position in the dental arch19.
Foremost reports of the use of attachments for
overdentures date back to the beginning of this
century20,21. Integrating attachment retained overdentures into present dental practice will
open up a new dimension in everyday dental
treatment and enhance patient satisfaction13. Teeth,
that are planned for extraction because of their
questionable prognosis,can be considered as longterm or short-term alternatives to implant or total
edentulousness. For the success of an overdenture,
patient selection is crucial. The attitude of the
patient towards the treatment should be evaluated
and only those who can comprehend, both, the
benefits and the limitations of attachments ought to
be treated with attachment retained overdentures17.
The other significant prerequisite for the success of
overdentures is patient’s awareness of oral hygiene
and maintenance which includes exceptional
oral care at home with professional aid in order
to prevent failures22,23.
It is impossible to overemphasize the necessity
for simple attachments for overdenture fixation.
Snap fasteners or stud-type attachments, are
simple in idea and use. Some stud attachments
are resilient and have a spring return (Gerber).
Others are tissue resilient (Dalbo); the few others
are non-resilient (Introfix). Resilient attachments
can either be unidirectional or multidirectional.
Resilient attachments have a compensating
mechanism where they allow the tissues to support the denture base, rather than the tooth;
this feature act as a safety regulator in the event
of an overload24. Therefore, In the present report a
ball type of resilient stud attachment system was
used. A resilient attachment was chosen in-order
to enhance the retention, as the patient initially
reported to us with a complain of ill-fitting denture
and an O-ring does not transfer load onto the
tooth/root, rather it acts as a retentive device. The
O-ring system is thought to be the best attachment
as it acts passively on the abutment teeth25. They
provide satisfactory retention, are easy to use in
terms of insertion and removal and comfortable
for the patient17. To evaluate the retention of an
O-ring attachment system at different degrees
of inclinations, Rodrigues et al26 conducted a
study. According to them O-ring stud placed
perpendicular to the occlusal plane demonstrated
satisfactory retention during the course of first
year; they also found that the retentive capacity of
the O-ring was affected by inclination of the stud,
O-ring stud perpendicular to the occlusal plane
were show to have highest retention. Hence, inorder to achieve parallelism between the studs a
surveyor was used, in the present report, to position
the studs without any inclinations [Fig.12 & 13].
According to literature, impaired dental status
causes dietary restrictions due to difficulty of
inability to chew, thus resulting in diminished
nutritional status27-29. Of those who are over 65
years of age, 60% are totally edentulous, and on
the average, they experience a 70% loss in chewing
efficiency when compared to patients with natural
teeth. This reduction in chewing ability has a
significant effect on the dietary preferences of these
patients and it has been reported that patients
over the age of 70 have a consistently inadequate
nutritional intake30. Rissin and co-workers, in
their study compared the masticatory efficiency
in patients with natural dentition, complete denture
and over denture. They concluded that patients
wearing overdenture had a chewing efficiency onethird greater than the complete denture patients31. Although overdenture has numerous advantages,
some of their disadvantages are that the prosthesis
tends to be bulky and over contoured. Patient
selection is very important as maintenance of
oral hygiene is of utmost importance in order to
prevent caries, periodontal disease, and failure of
abutment teeth. The other drawbacks are that, they
cannot be used in patients with bony undercuts.
Overdenture tends to encroach on the inter-occlusal
space12 which can cause reduction in freeway
space if not planned properly. This treatment
modality will require frequent recall check-ups and
relining procedure as resorption in the posterior
part of the arch will continue.
With time, lack of retention can be a common
grievance in complete denture patients. Although in
recent years implant supported overdentures have
gained popularity, they may not be affordable to
all patients. In such case, tooth borne overdenture
can be advised. Incorporation of attachments
in overdentures elevates modest overdenture to
another level by adding mechanical retentive
properties. The O-ring is one such stud attachment.
Various materials such as waxes, resins, acrylic
can be used for casting. Our technique offers a
simple and alternative technique, to the current
method, for the fabrication of stud attachment.