Abstract:
Obstructive sleep apnea (OSA) is the most common
sleep-related breathing disorder with periodic
reduction or cessation of airflow during sleep.
Prevalence of obstructive sleep apnea is favored
in men more than woman. Risk factors include
nasal obstruction, obesity, gender, craniofacial
anatomy, and smoking. Polysomnography is proved
to be the golden-standard method for diagnosing
obstructive sleep apnea. Treatment of OSA varies
from simple measures such as oral appliances and
nasal continuous positive airway pressure (CPAP)
to surgical procedures. Oral appliance, namely,
mandibular advancement device (MAD) is the
recommended treatment appliance for the patient
with mild to moderate OSA. For the dental profession
in general and in prosthodontists speciality, the
subject of sleep medicine continues to offer great
challenges and opportunities in diagnosis, treatment
planning, and treatment based on qualitative
evidence. This article discusses the various aspects
and prosthodontic perspectives of obstructive sleep
apnea in detail.
Key words: Obstructive sleep apnea, predisposing
factors, symptoms, polysomnography, oral
appliances.
Introduction
Obstructive sleep apnea is the most common
respiratory disease associated with chronic
insomnia.1
OSA is defined as the condition
of repetitive episodes of complete or partial
collapse of the upper airway during sleep that is
followed by transient awakening, which results
in restriction of the upper airway permeability.2
Airway obstruction can occur in many areas of
the nasopharynx, oropharnyx, and hypopharynx.
The severity of OSA is expressed as the Apnea
Hypopnoea Index (AHI). It is the number of apneas
and hypopneas per hour of sleep. Due to the
multifactorial nature of this condition, management
includes a multidisciplinary approach.3
The role
of prosthodontists is becoming more significant in
treating sleep disorders especially in patients with
mild to moderate obstructive sleep apnea (OSA).1
They should recognize the signs and symptoms
of OSA, refer to the physician for diagnosis, and
collaborate with the health team surrounding the
patient in providing care that will improve the
patient’s oral and general health.4
Epidemiology:
It has been reported that 10% and 5% of men
and women, respectively, in the 30–40-year age
group are common snorers, reaching at least
20% for males and 15% for females in the 50-60
year age group. It has been reported that 5% of
the world population is affected by OSA, with the
prevalence of 4% for men and 2% for women in
the age of 30-60 years.1
Predisposing factors:
Obesity is an important risk factor for obstructive
sleep apnea (OSA). Among the severely obese,
the prevalence of OSA ranges from 55% to 100%.
Craniofacial anomalies like micrognathia and
retrognathia, enlarged palatine tonsils, enlarged
uvula, high-arched palate, nasal septal deviation,
longer anterior facial height, steeper and shorter
anterior cranial base, inferiorly displaced hyoid
bone, disproportionately large tongue, a long soft
palate, and decreased posterior airway space
also predispose to obstructive sleep apnea.5
In addition to age, genetic, ethnic and gender
predilection and various habits such as alcohol
consumption, smoking and drugs use, the existing
OSA is aggravated.1
Pathophysiology:
The upper airway is a soft tissue tube, the patency
of which is maintained, in part, by muscles such
as tensor veli and genioglossus. The base of the
tongue obstructs the upper airway resulting in
snoring. The upper airway is composed of the
nasopharynx, oropharynx, and hypopharynx.
When the patient falls asleep in the supine position,
muscle relaxation causes the base of the tongue to
approach the posterior wall of the pharynx. With
the consequent reduction of airflow, the patient
must increase the airflow speed to maintain the
required oxygen supply to the lungs. This increase
in airflow velocity causes the vibration of soft
tissues that produces snoring.1
Symptoms:
The clinical features of obstructive sleep apnea
are memory problems, excessive day time
sleepiness, poor concentration, night drooling
of saliva, depression, irritability, xerostomia,
poor work performance, occupational accidents
and a reduction in social interactions. OSA is
associated with hypertension, ischemic heart
disease, heart failure, cerebral ischemia, and
cardiac arrhythmias.5
Investigations:
The procedures followed in diagnosing a patient
with OSA are few but precise. These methods
include a polysomnography test and a home sleep
apnea test. Both of which are sleep studies, the
most effective and accurate diagnostic tools.2
- Polysomnography: This testing
method is deemed as the gold standard
examination to diagnose OSA.6
The test
involves overnight recording of sleep,
breathing pattern, and oxygenation. The
study records analysis of apnoea, oxygen
saturation, body position, change heart
rate, snoring, desaturation relations, and
sleep staging.1
- Lateral cephalogram: It is useful
to analyse skeletal and soft tissue
characteristics of patients with OSA and
has the advantage of being available in
most dental clinics, easy to perform and
less expensive.7
- Magnetic resonance imaging:
Dynamic MR imaging can accurately
diagnose the cause and level of upper
airway narrowing in patients with OSA.
It can characterize and anatomically
classify the level of narrowing for planning
reparative surgery.8
- Computed tomography: CT scanning and MRI significantly improves soft tissue
contrast and allows precise measurements
of cross-sectional areas at different levels,
as well as three dimensional reconstruction
and volumetric assessment. CT scanning
has provided valuable insights into the
pathophysiology of Sleep Disordered
Breathing and plays a major role in its
management.5
- Acoustic reflection test: It provides
an objective measurement of the nasal
and pharyngeal cavities.9
In this test, the
sound wave is projected into the airway
and is reflected back through the tube
to a computer which creates graph that
determines the location of the obstruction.5
Diagnosis:
The diagnosis must be made by a sleep physician.
The role of the prosthodontist is to screen patients
using the Epworth Sleepiness Scale, Stopbang and
Berlin assessment tools and an oral examination
and refer the patient to a sleep physician for
diagnostic and treatment prescription when OSA
is suspected.4
Patient history regarding frequent
awakenings, difficulty falling asleep, unrefreshing
sleep, daytime sleepiness, mood disturbances,
reduced motivation, morning headaches, excessive
nocturia has to be taken5
and proper physical
examination has to be done.
Treatment:
Treatment of sleep-disordered breathing can
be divided into following categories general
categories. These include: (1) Lifestyle modification
i.e. weight loss, cessation of alcohol consumption,
sleep position training, (2) Positive airway pressure
(CPAP), (3) Positional therapy, (4) Oral appliances
and (5) Upper airway surgery.2
Lifestyle modification:
Patients with OSA and comorbid obesity should
be counselled on long term weight management. A goal BMI<25 kg/m2 through dietary or surgical
weight loss may improve the AHI in obese patients
with OSA.10
Positive Airway Pressure Treatment
- Continuous Positive Airway Pressure
(CPAP): The first line treatment for mild-severe OSA patients is CPAP. It had been
discovered in 1983 by Dr. Sullivan. CPAP
has constantly been demonstrating that it
reduces the nocturnal obstructive events
from the first night of the treatment.11 ”CPAP
introduces a column of air that serves as
a pneumatic splint for the upper airway
preventing the airway from collapsing
that is the physiological definition of the
syndrome”.12 Due to the mechanism of
CPAP, it has been proven that it eliminates
snoring while sleeping. Therefore, CPAP
is considered to improve quality of life by
reducing OSA symptoms.13 Individuals
with pressure intolerance may experience
dryness or irritation of nasal and pharyngeal
membranes, nasal congestion or eye
irritation from air leakage with CPAP use.
- Bilateral PAP: It provides two different levels
of pressure and can potentially treat OSA
at a lower mean pressure than CPAP, at the
same time improving lung ventilation via a
pressure support. Bilateral PAP is a valid
alternative in patients intolerant to CPAP.14
- Autotitrating CPAP: It is a more sophisticated
device providing an alternative to traditional
CPAP. Auto CPAP continuously and
automatically adjusts the delivered pressure
in order to maintain upper airway patency
following changes in airflow resistance.
Compliance with Auto CPAP is slightly higher
compared with fixed CPAP.14
Positional therapy:
PT, a device that prevents patients from lying on their back, is considered as an alternative
treatment for milder OSA patients. PT has many
forms, such as the tennis ball technique. This
technique consists of a small ball that is attached
on the posterior part of the patients to obstruct
sleeping on a supine position. Supine alarms and
different positional pillows also improve the OSA
symptoms respectfully. Although PT is effective
and well tolerated in mild OSA cases, it remains
an inferior treatment when compared to CPAP.15
Surgical options:
- Classic procedures that directly enlarge the
upper airway,
- Specilaized procedures that enlarge the upper
airway by modifying soft tissue elements and/or
the skeletal anatomy,
- Tracheotomy for control by means of bypassing the pharyngeal portion of the upper airway. Most
procedures tend to address either the retropalatal
or the retrolingual portion of the pharyngeal
airway.16
Oral appliances:
Oral appliances were first referred to in 1923 in
books by the French paediatrician Pierre Robin,
who described the fall of the tongue base as
a cause of nasopharyngeal impairment and
suggested a prosthesis.17 They were started
using after describing a tongue retaining device
to treat snoring and apnea by Cartwright and
Samelson.18 A renewed interest followed this device
in mandibular development devices (MADs) that re-positioned the mandible in the protrusive position
to help maintain the patency of the upper airway
during sleep. The appliances can be broadly
classified into the following types:
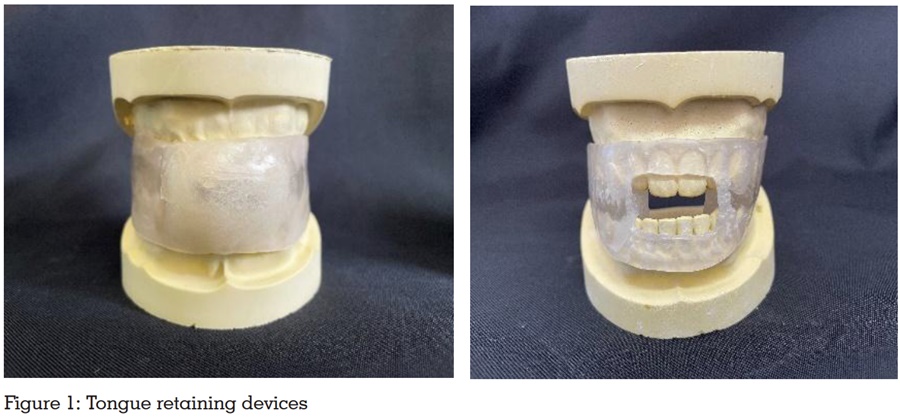
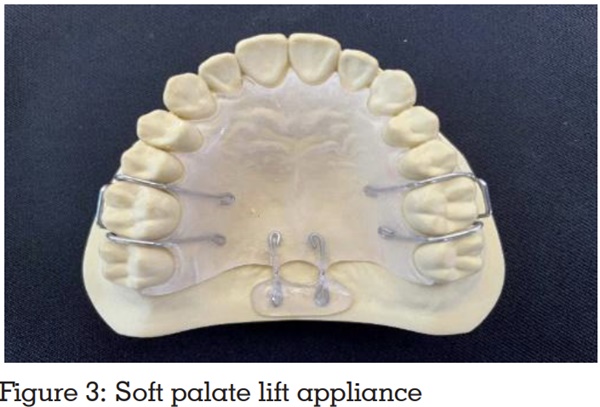
- Tongue-retaining devices (TRD): TRDs
incorporate an anterior hollow bulb, which
generates a negative pressure vacuum when
the tongue is inserted (fig 1). The tongue
is held forward, away from the posteriorpharyngeal wall, opening up the airway.
Owing to muscle anatomy, this appliance
simultaneously modifies the position of
the mandible. These devices are indicated
for edentulous patients, and patients with
potential temporomandibular joint problems.
TRDs do not require retention from dentition,
Minimal adjustments are required, Cause
minimal sensitivity to teeth and TMJ.1
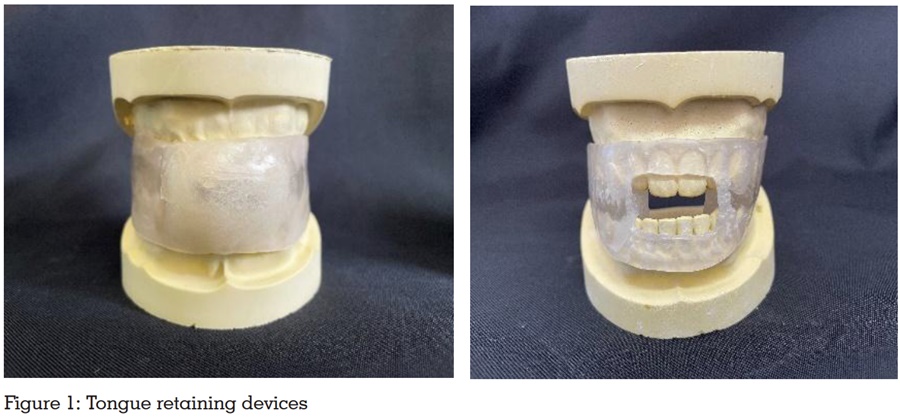
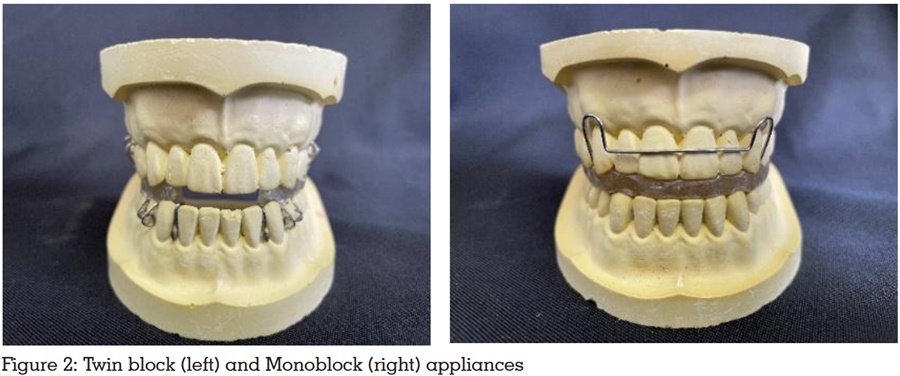
- Mandibular advancement devices (MAD):
It advances the mandible, brings forward
the tongue and other muscles of the pharynx
and elevates the palatoglossus muscle;
thus, airway patency is enhanced. It also
holds the mandible and other structures
in a stable position to prevent the mouth
opening. This is usually the most widely
used respiratory device for apnea and has
a higher evidence base. The devices cover
the upper and lower arch and have metal
hinges. The mandibular advancement
device requires good retention, sufficient
protrusion to maintain airway, minimal
vertical opening, and full occlusal coverage.1
Reduced effectiveness in patients with: TMJ,
myofascial pain, tooth tenderness, excessive
- PM positioner: This appliance links the
upper and lower splints with bilateral
orthodontic expanders. This appliance is
made of thermoplastic material that must be
heated in hot tap water every night before
it is placed in the mouth.20
- Elastic mandibular advancement (EMA):
It is the thinnest and least bulky of all the
appliances. It is similar to clear acrylic
orthodontic retainers, and moves the jaw
forward in fairly significant steps, and can
be difficult to tolerate.5
- Klearway oral appliance: The Klearway
oral appliance uses a maxillary orthodontic
expander to move the mandible forward
sequentially. Klearway is a fully adjustable
oral appliance used for snoring and mild
to moderate OSA. A Small increase in
mandibular advancement is initiated by
the patient, preventing rapid jaw movements
that cause significant patient discomfort.21
- The Thornton adjustable positioner
(TAP): This enables the progressive 0 mm
advancements of the jaw through the anterior
screw mechanism at the labial aspect of the
upper splint. This appliance has a separate
section for both the mandible and maxillary
jaws.22
- Modified Herbst Appliance: This design links
upper and lower splints with a piston post
and sleeve adjustable telescopic mechanism
on each side. It prevents side to side motion,
but since the mandible is held close with
small orthodontic rubber bands, opening
the jaws is fairly easy.5
- DUOBLOC: It is a Custom-made adjustable
mandibular advancement device (MAD) for
the treatment of obstructive sleep apnea
(OSA). This MAD has attachments in the
frontal teeth area that allow for progressive
advancement of the mandible.5
- The silencer system: This incorporates
titanium precision attachments at the incisor
level, allowing sequential 2 mm advancement
of up to 8 mm, lateral movement of 6 mm,
(3 mm bilaterally) and vertical pin height
replacements. It is the only appliance
that enables anteroposteriorly adjustment
and an open and closed position since it
includes a very expensive titanium metal
hinge device.23,24
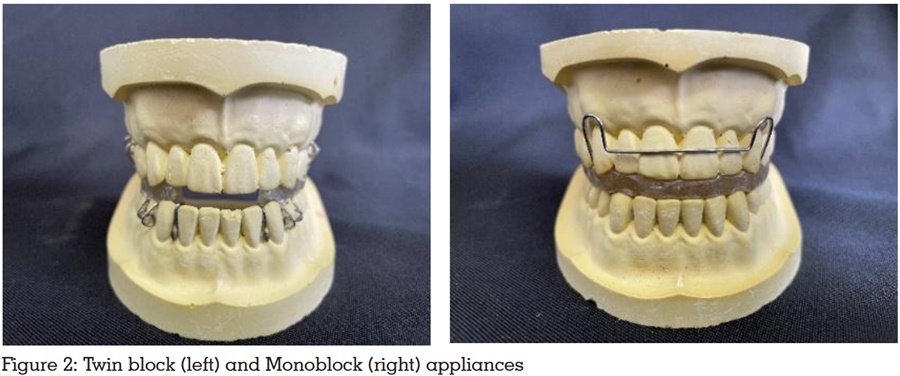
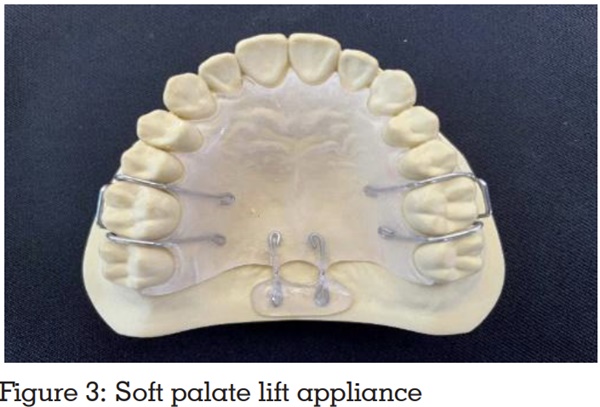
- Soft palate lifting: The soft palate lifting
prosthesis lifts and/or stabilizes the soft palate,
preventing vibration during sleep (fig 3). The
palatal lift prosthesis significantly improved the
upper airway passage and eliminated snoring
and airway obstruction, and improved the patient’s
overall quality of life.25
CONCLUSION
Over the last decades, studies conducted on
OSA have noted its prevalence and revealed
its various risk factors, associated symptoms,
successful diagnostic means, and effective therapy
options.2
Untreated sleep apnea is one of the
major public health issues we face in common.
Oral appliances play a crucial role in managing
non-surgical OSA and have become the first line
of treatment for almost all patients with OSA.
The emergence of dental sleep medicine as a
safe and effective treatment brings hope for the
millions of patients looking for alternatives to
CPAP treatment. Oral appliances used till date
constitute a relatively heterogeneous group of
devices for the treatment of sleep apnea and non-apneic snoring. Prosthodontists play a pivotal role
in the initial diagnosis, management, and care of
patients with sleep apnea.
REFERENCES
- Cheruku S, Duggineni CR, Harilal G, Lukka P. Obstructive
sleep apnea: oral appliances and materials. Int J Dent
Mater 2021;3(2): 58-63.
- Johar RA et al.. Obstructive Sleep Apnea: A Review
Article. Saudi J Oral Dent Res 2021;6(5): 221-226.
- Nayar S and Knox J. Management of obstructive sleep
apnea in an edentulous patient with a mandibular
advancement splint: A clinical report. J Prosthet Dent
2005;94(2):108-111.
- Wu JC and Dubois NMG. Role of Oral Devices in
Managing Sleep-disordered Breathing Patients. ACP
2016;1-7.
- Chandra SD, Raj KS, Prema et al. Obstructive sleep
apnea and its prosthodontic management- an overview.
Int J Health Sci Res. 2018; 8(3):259-265.
- Maspero C, Giannini L, Galbiati G, Rosso G, & Farronato G. Obstructive sleep apnea syndrome: a literature review Minerva Stomatol 2015; 64(2):97-109.
- Gungor AY, Turkkahraman H and Yariktas M.
Cephalometric comparison of obstructive sleep apnea
patients and healthy controls.Eur J Dent. 2013;7(1):48-54.
- Bhawa, santhosham R, Anand S and Joseph S.Role of
dynamic MR imaging in obstructive sleep apnea. Indian
J Otolaryngol Head Neck Surg.2008;60(1):25-29.
- Viviano JS. Acoustic reflection: Review and Clinical
Applications for Sleep-Disordered Breathing. Sleep and
Breathing. 2002;8(3).
- Pavwoski P and Shelgikar AV. Treatment options for
obstructive sleep panea. Neurol Clin Pract 2017;7(1):77-
85.
- Spicuzza L, Caruso D and Di Maria G. Obstructive sleep
apnoea syndrome and its management. Therapeutic
advances in chronic disease. 2015;6(5):273-285.
- Weaver T. E, Calik M. W, Farabi S. S and Fink A. M et al.
Innovative treatments for adults with obstructive sleep
apnea. Nature and science of sleep. 2014;6.
- Donovan L. M, Boeder, S Malhotra A and Patel S. R. New
developments in the use of positive airway pressure for
obstructive sleep apnea. Journal of thoracic disease.2015;
7(8).
- Spicuzza L, Carusa D and Maria GD. Obstructive
sleep apnea and its management. Adv Chronic Dis.
2015;6(5):273-285.
- Weaver T. E, Calik M. W, Farabi S. S, and Fink A. M.
Innovative treatments for adults with obstructive sleep
apnea. Nature and science of sleep 2104;6:137.
- Padma A, Ramakrishnan N and Narayanan V. Managemnt
of obstructive sleep apne: A dental perspective.
2007;18(4):201-209.
- Robin P. A fall of the base of the tongue considered as a new cause of nasopharyngeal respiratory impairment:
Pierre Robin sequence, a translation. Plast Reconstr
Surg 1994;93(6):1301-3.
- Cartwright RD, Samelson CF. The effects of a nonsurgical
treatment for obstructive sleep apnea: the tongue-retaining device. JAMA. 1982;248(6):705-9
- Doff MH, Finnema KJ, Hoekema A, et al. Long-term oral
appliance therapy in obstructive sleep apnea syndrome: a
controlled study on dental side effects. Clin Oral Investig
2013;17(2):475–82.
- Giannasi LC, de Mattos LC, Magini M, Costa MS, de
Oliveira CS, de Oliveira LV. The impact of the Adjustable
PM Positioner appliance in the treatment of obstructive
sleep apnoea. Archiv Med Sci. 2008;4 (3):336.
- Lowe AA. Titratable oral appliances for the treatment of
snoring and obstructive sleep apnea. J Can Dent Assoc
1999;65:571-4.
- Thornton WK, Roberts DH. Nonsurgical management of
the obstructive sleep apnea patient. J Oral Maxillofac
Surg. 1996;54(9):1103-8.
- Wade PS. Oral Appliance Therapy for Snoring and Sleep
Apnea: Preliminary Report on 86 Patients with an Anterior
Mandibular Positioning Device, The Silencer. Journal of
Otolaryngology. 2003;32(2).
- Schönhofer B, Stoohs RA, Rager H, Wenzel M, Wenzel
G, Köhler D. A novel tongue advancement technique for
obstructive sleep apnea and snoring: Side effects and
efficacy. Am J Respir Crit Care Med. 1997;155:732-8.
- Bhalla G, Arya D, Chand P, Singh K, Tripathi S.
Management of obstructive sleep apnea with a palatal
lift prosthesis. International Journal of Stomatology and
Occlusion Medicine. 2013;6(3):101-5.