The quality of life after rhinectomy is severely compromised if an efficient surgical reconstruction or a prosthetic device is not provided. Sometimes the results of the plastic surgery are not sufficient to restore the entire volume of the nose .In these patients, a facial prosthesis is aesthetic and provides the respiratory function. Introduction of new material which gives life-like appearance to such prosthetic restorations e.g. silicone and poly ether rubbers have given a new dimension to rehabilitation of such patients. This report presents a case of prosthetic rehabilitation of the nasal component of the face secondary to partial rhinectomy for squamous cell carcinoma. Rehabilitation of patient was done by mechanically supported prosthesis using spectacles. Patient’s aesthetics and respiratory function has been significantly improved following prosthetic rehabilitation.
Key words: nasal prosthesis, silicone, spectacles.
Facial defects resulting from neoplasm, congenital
malformation or trauma can be restored with facial
prosthesis to achieve life-like appearance and
function. Facial prosthesis demands a seamless
harmony of art and science for accomplishing
perfection. The texture, form and color of the
prosthesis should closely resemble the patients
missing facial structure so as to make it extremely
difficult for a spectator to discriminate between the
two. The quest for identifying the best means to
achieve such resemblance has made maxillofacial
prosthetists to try a vast array of materials and
techniques for the fabrication of facial prosthesis.
Facial defects secondary to treatment of neoplasms
result in multiple functional and psychosocial
difficulties requiring surgical reconstruction
techniques, prosthetic rehabilitation or a
combination of both these methods to restore the
associated facial disfigurements. This helps to
improve the level of function and self-confidence
of patients.1
A nasal prosthesis can bring back esthetic form
and anatomic contour for mid-facial defects, often
more efficiently than surgical reconstruction since
the nose is a relatively immobile structure. For
successful camouflage of the defect , lot of factors
such as harmony, texture, color matching and
merging of the prosthesis with tissue interface
are important. The aim of the presented case
report is to describe the non-surgical rehabilitation,
with silicone nasal prosthesis for a patient who
had undergone partial rhinectomy as part of the
treatment for squamous cell carcinoma of nose.
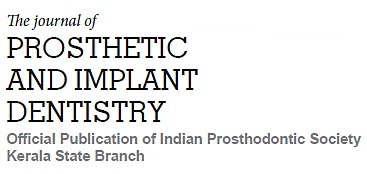
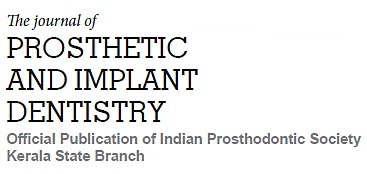
A 77 year old male reported to the Department of
Prosthodontics, GDC, Kottayam for replacement of nose which was surgically excised for treatment
of squamous cell carcinoma. He had undergone
partial rhinectomy and radiotherapy as part of
the treatment regime and a post radiation vitiligo
had developed around the nose. The defect was
found to involve the entire right side of the dorsum
of nose extending from lower one third of nasal
bone including lateral nasal cartilage and alar
cartilage and extending up to anterior nasal
spine of maxilla . Left half of the nose was also
deformed. (fig 1) On examination, the patient
expressed dissatisfaction with his appearance
and was especially concerned about the facial
disfigurement. Various prosthetic treatment
modalities ranging from acrylic resin nasal
prosthesis to implant retained silicone prosthesis
were explained and discussed with the patient.
Considering all the factors, fabrication of silicone
nasal prosthesis was planned, and the outcome
of this treatment was explained to the patient. It
was decided to utilize anatomic undercuts and a
spectacle glass frame for retaining the prosthesis.
Squamous cell carcinoma is an aggressive
malignant neoplasm. The quality of life after
rhinectomy is severely compromised if an efficient
surgical reconstruction or a prosthesis is not
provided.2
Prosthetic management of nasal defects
that result from trauma or surgery has been well documented. The literature indicates that 3 to 5
months of post operative healing may be required
to allow for contraction and organization of the
tissue bed before commencing fabrication of a
definitive nasal prosthesis.3
The advantages of
nasal prosthesis are that it is inexpensive, easy
to fabricate, esthetically good, can be given in
healing phase and most importantly recurrence
can be observed easily after the malignant tumor
resections.4
Anatomic undercuts, secondary
mechanical factors, skin adhesives, and implants
(Magnets or Osteointegrated implant retained
titanium screws) are reported to provide sufficient
retention.5,6
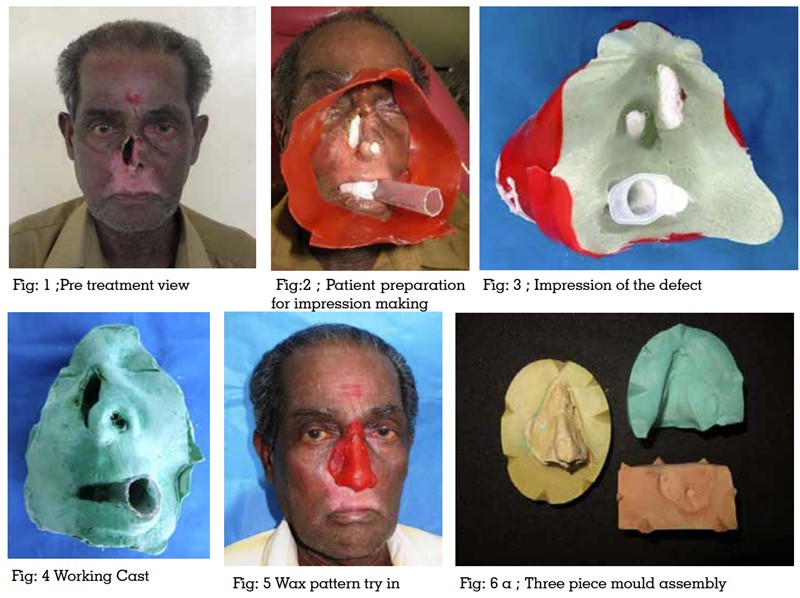
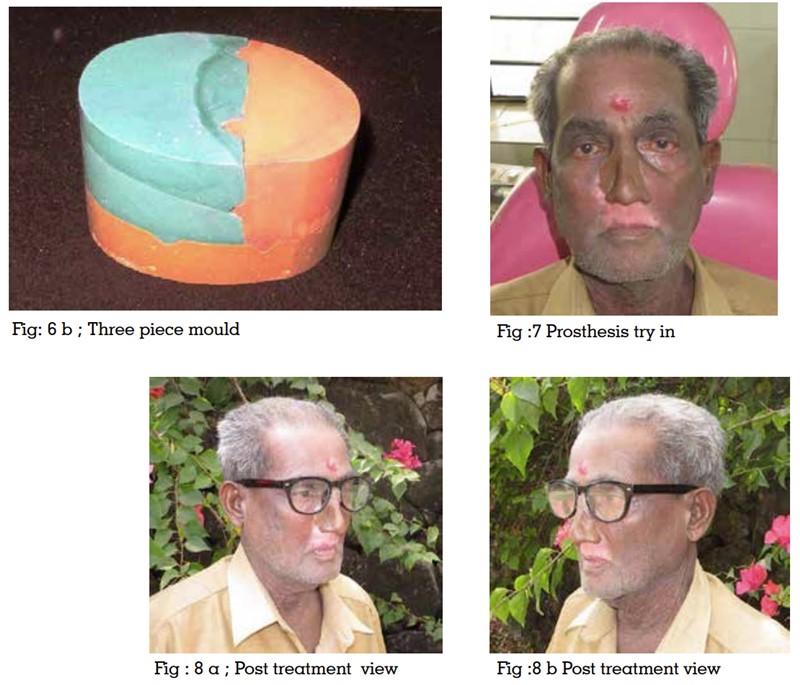
The current prosthesis was made to restore the
esthetic appearance of the patient which utilized
anatomic undercuts for retention with an additional
mechanical retention utilizing a spectacle glass
frame without inserting craniofacial implants.
In this case report, anatomic undercuts and
spectacles were used for retention and silicon
material was used for the fabrication of nose
prosthesis as it seemed to be adequate to maintain
both the texture and the appearance of natural
tissues.7,8 Surface details and characteristics can
be modified using intrinsic and extrinsic coloration.
In this case, both intrinsic and extrinsic coloration
was preferred as it was permanent and esthetically
superior. The patient’s esthetics, confidence and
satisfaction were tremendously improved by such
nasal prosthesis.