Dental implants have been used for replacement of missing teeth. Various factors are considered to determine the success rate of dental implants. One of the important factors determining the success rate is peri-implant bone loss that occurs subsequently after implant placement. A variety of etiological factors have been listed responsible for peri-implant bone loss. One among the etiological factors for bone loss pertaining to implant geometry is implant-abutment connection type. Implant abutment connection type should be designed to minimize the bone loss around implants. Hence it is important to analyze and compare the bone changes that occur around implants with different connection types to choose an appropriate type for achieving maximum success rates.
Key words: Peri-implant bone loss, implant-abutment connection, internal hex, external hex, platform switching, morse taper.
Dental implant restoration is currently widely
practiced treatment modality for replacement of
missing teeth and to restore human masticatory function. Long term success of dental implants
depends on successful osseointegration, bone level
stability and maintenance of soft tissue health1.
Albrektsson et al proposed that a dental implant
is considered successful if peri-implant crestal
bone loss is less than 1.5 mm during the first year
after implant placement and less than 0.2mm annually thereafter2
.
Peri-implant bone remodeling occurs after the
implant is exposed to oral environment during
second stage surgery or when abutment is placed
immediately following implant placement. Remodeling process causes marginal bone resorption
which is affected by variety of factors such as
traumatic surgical technique, excessive loading,
implant -abutment micro gap ad its microbial
contamination, biologic width reestablishment,
peri-implant inflammatory infiltrate, micromovements, repeated screwing and unscrewing and
implant neck geometry3
.
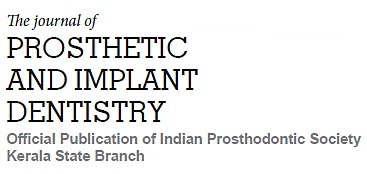
The type of implant -abutment connection (IAC) is
one of the major factors which affects the crestal
bone level changes. Implant abutment interface
should be designed to reduce stress on prosthetic
component and on bone-implant interface by incorporating features of anti-rotation and should be able to resist bacterial penetration4. The IAC
can be of external connection which has standard
geometric projection on the implant platform or
internal connection where mating components are
recessed into implant body5
(Fig 1 – a & b). IAC can
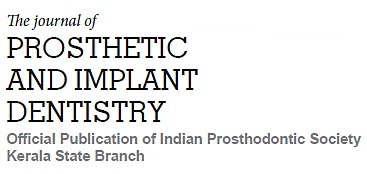
be further characterized as a slip fit joint where
slight space exists between the mating parts e.g.
external or internal hex, or a friction fit joint where
mating components are literally forced together
e.g. Morse taper (Fig 2) and cone screw connection4
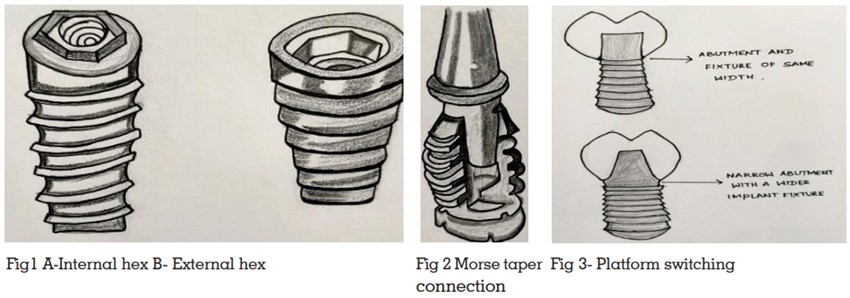
. One potential way to reduce marginal bone
loss is to physically move the implant-abutment
interface horizontally using smaller diameter abutments to connect to implants. The manufacturers
changed the configuration from butt-joint to an
internal cone connection combined with nonmatching implant and smaller diameter abutment.
These types of connections have been termed as
Platform switched connections6
(fig 3).
The objective of the present study is to review the
predictable marginal bone loss around dental
implants with different implant-abutment interfaces
using the available evidence.
Initial 0.7mm tall external hex connection with a
butt joint was introduced by Branemark. It was
found to have reversibility and compatibility with
different systems4
. It was designed to provide
a rotational torque transferring mechanism for
implant placement and later evolved by necessity into a prosthetic indexing and anti-rotational
mechanism6. But in external hexagon there is
existence of a microgap in the implant-abutment
interface7. Major drawback was screw loosening
and fatigue fracture due to short hex height and
limited engagement which lead to micromovements and joint instability4. Placing an abutment
on submerged implant with external hexagon
created a butt-joint interface between the implant
and abutment. Many experimental and clinical
studies documented that marginal bone loss occurred around these implants6.
In a study by Herman et al, tissue-level (nonsubmerged implant) was used as control and experimental group included models with presence of
an interface (microgap) at the implant-abutment
interface. This study was able to demonstrate
1.5-2.0 mm bone loss around bone level, external hexagon butt joint implants when there was
an interface created (at 2nd stage surgery) or
immediately if the abutment was placed on the
implants. When no interface existed as in tissue
level implants (control group), no or minimal bone
loss was observed. Further if the interface was
moved apically, more bone loss occurred and if
the interface was moved coronally, less bone loss
was observed6
. According to study by Hartman
and Cochran amount of bone loss was related
to location of interface, relative to the crest of the
bone. The closer the interface to original bone
level, the more bone loss was observed8
. This was
common finding around butt-joint connections
and approved by many others6
. The hypothesis
for the bone loss around these implants was related to the presence of bacteria in the interface
between implant and abutment connection. As
in external-hexagon butt joint implant systems,
a contaminated micro-gap exists in the interface,
prevention of microbial leakage has been challenging for restoration of two staged implants to
minimize inflammatory reaction and maximize
the bone stability around implants6.
This interface was developed to overcome clinical
complications of external connection. Initial internal connection introduced by Niznick had 1.7mm
deep hex below 0.5mm wide, 45 degree bevel4
.
The mating components are deep within implant
body which shifts the implant abutment fulcrum to
the middle of the implant resulting in better stress
distribution and prosthetic screw stability. Main
advantage is the long internal wall engagement
body, resisting micromovements at the implant
abutment interface. Levin noted screw loosening
incidence as low as 3.5 %. Weaker link in internal
connection is bone rather than prosthetic screw as most of the stress concentrates in the bone
around implants4
.
Through the years, internal connections have
evolved into numerous designs in an attempt to
achieve better microbial seal and joint stability.
Internal slip fit connections having an internal
geometrical anti rotational feature like hexagon,
octagon, spline or trichannel are marketed now4
.
Internal conical connection /Morse taper (cone
within cone) has conical projection from the abutment tightly fitting into conical recess in the implant
body. Mechanical friction between external conical wall of abutment and internal wall of implant
locks them into cold welded stability eliminating
rotation and subsequent screw loosening and
also allows for even distribution of stress with the
implant, abutment and screws9,10. Screwing torque
required is less compared to external and internal
hexes and also provides adequate biological seal4.
According to systematic review by Riccardo et
al peri-implant bone loss in implants having an
internal or conical connection was less compared
to implants with external hexagons. The internal
and especially conical connection was found to
be maintaining stable crestal bone levels in the
short – medium period. The reason for better results
observed for conical connections is because of
reduction in micro-gap and reduced micromovements during loading1. Few studies revealed there was significant difference in peri-implant bone
loss between external and conical connections.
However, it was less evident for internal and conical ones5
Rodrigo et al stated that osseointegrated implants
with internal connections showed less marginal
bone loss as compared to external connection implants. This is mainly due to presence of platform
switching present in internal connection implants.
This is because in platform switching, the
implant abutment connection is far away from the
margin, which causes decreased load concentration, decreased micro movements and bacterial
colonization takes place at a farther region of
bone11.
One theory stated step created between abutment and implant allows the biologic width to be
established horizontally and less vertical bone
resorption is required to compensate for biologic
seal. Significant decrease in crestal bone loss was
found if implant abutment diameter difference
was greater or equal to 0.4mm4
.
Ericsson et al depicted the role of inflammatory
cell infiltrate for reduced bone loss. The physical
repositioning of implant-abutment connection from
external outer edge of the implant and bone may limit bone resorption by containing the inflammatory cell infiltrate within the angle formed at
the interface away from adjacent crestal bone6
.
According to results obtained from the systematic
review and Meta analysis by Momen et al inward
shifting of implant-abutment interface, by platform
switching can be considered desirable morphologic feature that prevents horizontal saucerization and preserve the vertical crestal bone levels.
Additional improvement in bone levels around
dental implants may be obtained with greater
degree of shifting3
.
According to canullo et al the marginal bone
around single platform switched implant placed
immediately and restored immediately showed
less resorption than non-platform switched implants. They also concluded that platform switched
implants placed and loaded immediately can
help in preservation of papilla by providing periimplant hard tissue stability12. Clinical relevance
of platform switching is more important in situations where anatomic structures like sinus floor
or alveolar nerve limit the residual bone height,
the platform switching approach minimizes bone
resorption and increases biomechanical support.
This review is to study the influence of the implant-abutment connection types on the marginal bone
level changes. With available evidence based on
various systematic reviews and meta- analysis
it can be concluded that 1.5 to 2mm bone loss
invariably occurred around bone level external
-hexagon butt joint implants where the interface
is contaminated with bacteria. Many studies have
shown that peri-implant bone loss is generally
lower when internal type of interface was adopted especially conical connections seem to be
more advantageous. Platform switched implants
have shown less resorption compared to platform
matched implants which is particularly suitable
when residual bone height is a limiting factor for
implant placement.