AIM: The aim of the present case report is to make
a life like prosthesis using the remnant portion of
the remaining finger and also it should resemble
the unaffected finger of the other hand.
INTRODUCTION: The individuals life quality
depends on the state of being free from any illness
or injury. Loss of body structure due to any form
of illness or injury will affects the morale of the
individual. Finger is a more vital organ to perform
classic everyday function. Any defect in the finger
leads to a psychological setback. Prosthetic
rehabilitation with an artificial silicone prosthesis
is the most viable treatment option. The present
article discusses a prosthetic rehabilitation of the
index finger of the right hand using a customized
ring retained silicone prosthesis.
CASE REPORT: A 48 year old female patient reported
with a principal complaint of partially lost right
index finger. The patient had a history of traumatic
injury 5 years ago with no evidence of pain on
palpation. The treatment options suggested to the
patient were implant supported endoprosthesis or
a conventional silicone exoprosthesis. The patient
opted for a conventional custom made silicone
exoprosthesis due to financial concern.
CONCLUSION: Restoration of finger defects with
an artificial substitute is no more a challenging
procedure for a maxillofacial prosthodontist. So
when silicon finger prosthesis is prepared with
utmost care it can improve the life like appearance
and psychological support of the patient.
Key words: Finger prosthesis, Ring retained silicone prosthesis, amputated finger.
Prosthetics is the art and science that provides a
natural aesthetic appearance by replacing the
absent structures of the patient. Hands are the
important organ which helps to perform wide
range of precise and gentle activities. According
to the National Centre for Health Statistics,
physical injury accounts for >70% of upper limb
amputations of which the most common are partial
finger amputations1
. The most common causes of
finger amputation are trauma caused during road
traffic accidents, occupational injuries, degloving
injury, frostbite, gunshot injury. This can lead to
reduced grasp, strength and also psychological trauma2
. Rehabilitation of the lost finger is
usually done by fabrication of an endoprosthesis
with implants or an exoprosthesis. Though an
endoprosthesis is of better acceptance, it cannot
be used in conditions with bare nerve endings in
the amputation site3
. Silicone could be a suggestive
material in the fabrication of finger prosthesis4
.
This is a case report describing the partial finger
defect rehabilitated using a silicone exoprosthesis
retained by a customized ring.
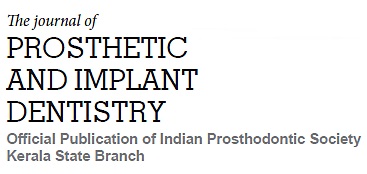
A 48 year old female patient reported to the
department of prosthodontics, with a principal
complaint of partially lost right index finger (fig .1).
The patient gave a history of traumatic crush injury
5 years ago during a road traffic accident due to which amputation was performed. On examination
there was complete amputation of distal phalanx of
the right index finger (Allen IV classification) about
2.5cm with solitary healed wound. On physical
examination there were no signs of inflammation
or infection. The tissue on the middle phalanx
was keratinised with brown to yellow crusting
.The dorsal and ventral surface was smooth and
rounded. The patient gave no evidence of pain on
palpation so the possibility of remnant free nerve
ending was negative. The patient do not have
any previous history of prosthesis. The treatment
options suggested to the patient was an implant
supported endoprosthesis or a conventional
silicone exoprosthesis. The patient was not willing
for surgical procedure and opted for a conventional
custom made silicone exoprosthesis.
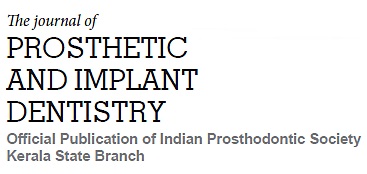
Before making the impression a thin layer of
separating medium, petroleum jelly was applied
to the patient’s hand. The impressions of both the
hands were made using irreversible hydrocolloid
(Zelgan plus, Densply, USA) using a broad plastic
container, which was selected based on the
patient’s palm size. Care was taken to place the
hand in relaxed position and without contacting
the bottom portion of the container while making
impression. The impression was poured with die
stone(Ultrarock, Kalabhai, India ) to produce
positive model of hand with amputated finger
(fig.2). Separate impression of the finger stump was
made using Putty elastomeric impression material
(Aquasil, Densply Pvt Ltd, Germany) and light body
elastomeric impression material (Reposil, Densply
Pvt Ltd, Germany)and a model was obtained by
using die stone (Ultrarock, Kalabhai, India ).
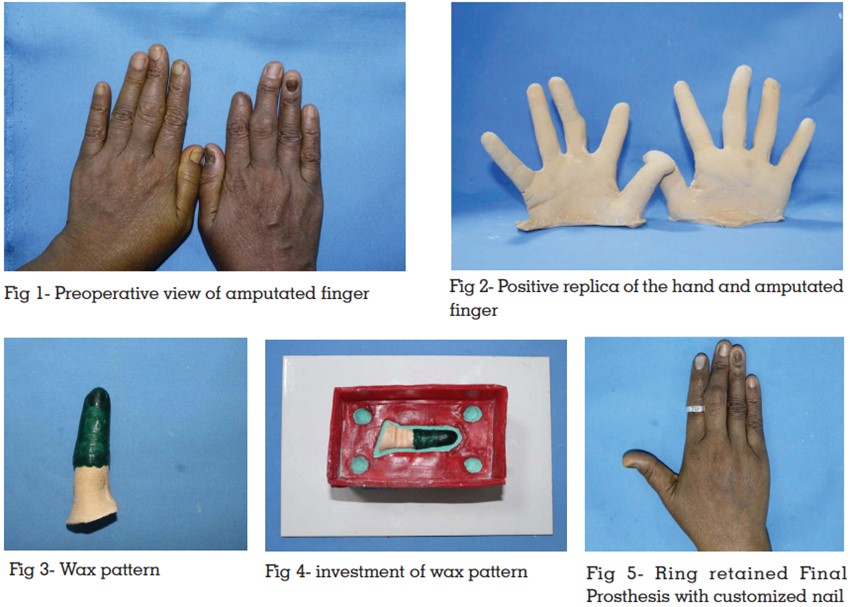
With the dimensions of the opposing finger as
reference a wax pattern was fabricated using
inlay wax (GC Asia Dental Pte Ltd, Singapore)
(fig. 3)and tried on the patient. After trial the wax
pattern was placed in refrigerator to prevent wax
distortion. Once the trial was satisfactory the finger
stump was reduced by 2mm with a rose head steel
bur (Morris dental company ltd, Dublin) in order to
attain a passive vacuum fit of the prosthesis. Then
the silicone was manipulated on a white tile and
a trial silicone sleeve was made on the reduced
finger stump to verify the fit. The trial sleeve had
sufficient vacuum. The trial sleeve was removed
from the finger stump and retentive grooves were
made using inverted steel vulcanite (Henry schein,
USA) on the dorsal and ventral surfaces of the
stump before mould preparation.
The previously tried wax pattern was then reoriented
in the finger stump and fused. Separating media
(DPI cold mould seal, DPI India) was applied in
the finger stump. A three part mould for silicone
packing was prepared using modelling wax (The
Hindustan Dental Products ,India) dental stone was
poured into the prepared wax mould and the dorsal surface of the finger stump was immersed into it
(fig 4). Grooves were made on the first counter for
reorientation. Separating media (DPI cold mould
seal, DPI India) was applied and a layer of wax
was placed on the counter to establish equalization
of pressure during silicone packing. The second
pour was done using dental stone. After the final
set of the three part mould, dewaxing was done.
Following dewaxing the mould was coated with a
layer of silicone releasing spray (Miracle Aerosol
industries, India). Finger nail of suitable shade
was fabricated and placed on the dorsal counter
in the mould using cyanoacrylate
A layer of separating media (DPI cold mould
seal, DPI India) was applied on the finger nail
section of the mould , then a thin layer of clear and
pink auto polymerizing acrylic resin (DPI RR cold
cure, DPI India) was poured in dough stage. After
polymerization the nail segment was removed
from the counter and trimming was done using
acrylic trimmers (shofu dental, India)
The manipulation of silicone (Technovent,
Macfacindia, India) was carried out on a neutral
white tile. Gradual addition of intrinsic satins
was performed for an evenly stained silicone
mass. Colour matching was done individually
for the dorsal and ventral sides of the finger. Once
the desired shade was achieved, silicone was
packed in increments on the both the counters. The
incremental addition of silicone was carried out to
eliminate entrapment of air bubbles that may lead
to voids. Then the counters were reoriented and
clamped for overnight curing for room temperature
vulcanization. Following the overnight curing the
prosthesis was removed from the stump and the
excess was trimmed by using sharp scissors.
The acrylic nail was removed from the silicone
finger and reattached with platinum primer (A304
Factor II, Inc, USA). The prosthesis was finished
by the burs which was provided in the kit by the
manufacturer. The prosthesis fit was checked on
the patient and final extrinsic shade matching was performed. In order to attain additional retention
and to camouflage the margins of the prosthesis
prefabricated metal ring was used (fig .5). Proper
postinsertion instructions were given for the patient
to maintain the finger prosthesis. Patient was
recalled after a week for review and patient was
highly satisfied and happy with the prosthesis.
Periodic follow up was followed for every three
months.
Defect or loss of a finger greatly affects the quality
of life of the individuals like ability to perform
function, dexterity of the hand is lost, the perception
of one’s wholeness is lost, the individual becomes
conscious to cloak himself in the society and if the
defect was due to a trauma or illness, may induce
symptoms of posttraumatic stress disorder (PTSD)5
.
Hence rehabilitation is necessary to regain the
physical and psychological wellbeing on the
patient.
Allen classified the amputation level for fingertip
amputations as Type 1 - injuries only involving
the pulp. Type 2- injuries involving both pulp and
nail bed. Type 3-injuries involving fracture of
distal phalangeal accompanying pulp and loss
of nail. Type 4- injuries involving the lunula, distal
phalanx, pulp and nail loss6
. The present case
report deals with a Type 4 Injury. Rehabilitation
of such defect can be done by reconstruction or
prosthetic rehabilitation.
Though advances in the microsurgical and
plastic surgical reconstruction techniques have
emerged, the reconstruction of the digits may not
be successful for all patients and so rehabilitation
has to be benefitted with a passive prosthesis.
Though the passive prosthesis cannot perform
function the purpose of prosthesis is to allow the
patient to camouflage in the society7
. According
to Michael et al scoring of the finger model could
improve the fitting of the prosthesis by mild compression of residual stump tissue8
. Silicone
was used in this patient as it has good strength,
lighter in weight, durable and provides more
esthetic appearance. Burkhardt et al had stated
that silicone has a property of hydration which
can improve the pliability and comfortability of
the hypertrophy scars9
. It can also protect and
desensitize the amputation region by providing
constant mild pressure over that area.
Retention of finger prosthesis can be enhanced by
ring, medical grade adhesives, implants etc10-12.
Patient’s normal hand can be used for fabrication
of wax pattern and the angulation can be modified
by sculpting. The major drawback of using silicone
elastomer is its color instability when it is exposed
to sunlight, chemicals, cosmetics and pollution. So
patient needs to be recalled after specific interval
to evaluate the prosthesis if required repair has
to be done. According to Pilley et al the rings
used for retention of finger prosthesis improved
the esthetics and psychological response of the
patient13. So ring retained finger prosthesis is said
to be a durable, simple, agreeable and inexpensive
treatment in developing countries when compared
to expensive options like implants.
In the present case, fabrication of prosthesis was
done with conventional silicone. The potential
benefits of using a silicone prosthesis are, they
desensitize the free nerve ending and protect the
finger stump from painful hypersensitive tissue by
applying gentle pressure constantly over the area
of amputation. As silicone prosthesis was found
to enhance the residual stump hydration, the scar
tissue becomes more pliable and comfortable14.
The finger prosthesis can be retained in the finger
stump by various modes, Larcher advocated the
usage of rings around the margins of the finger
prosthesis, adhesive medical grade adhesive,
Bickel KD used implant-retained endoprosthesis15-16.
In the present case retention was obtained using
a prefabricated ring placed on the silicone tissue
interface.
A suitable finger silicone prosthesis should have
appealing shape, merged margins, good fitting,
color matching to the adjacent skin, well contoured,
more detailed and aesthetic fingernails. It should
also restore the patient esthetics, function and
comfort. Restoration of finger defects with an
artificial substitute is no more a challenging
procedure for a maxillofacial prosthodontist. So
when care is given to prepare the silicone finger
prosthesis it can improve the life like appearance
and psychological support of the patient.
The effective method of using customized ring
retained silicon finger prosthesis could improve
the phycology, confidence level, retention and
aesthetics of the patient.