The application of vascularized fibula graft has become a standard methodology in the reconstruction of sizeable maxillo-mandibular defects. Fibula graft provides bi-cortical anchorage for dental implants. However, the mobile non-keratinized tissue on bone presents with proliferation after prosthetic intervention. The large prosthetic space also poses a challenge. Excessive height of the prosthesis above the implant platform creates a vertical cantilever that magnifies torque stresses on the crestal bone. This causes an overload on the implant-bone and the abutment-implant interface. Hence, there is a high chance of loosening or fracture of connecting screw. Increased prosthetic space makes it difficult for the patient to maintain oral hygiene. This paper presents cases with the prosthetic management of fibula reconstructed jaws with various types of implant supported prostheses that provide solutions to the above-mentioned challenges.
Key words: Mandibular reconstruction, free flap fibula, implant bar overdenture, vertical cantilever, resected mandible, hybrid denture
Large tumor resection and trauma in the head and neck region result in facial disfigurement and soft tissue mutilations. This results in unaesthetic facial forms and challenges in speech, mastication, and swallowing. The correction of the deformities of the maxilla and mandible can be done by surgical reconstruction. Prior to the introduction of microvascular reconstruction, conventional rehabilitation methods failed to re-construct the hard and soft tissues to satisfy anatomical and functional needs. Every reconstructive technique must satisfy the following key objectives:
Microsurgical methods have resulted in tremendous improvements in oral rehabilitation by re-establishing facial appearance. Vascularized bone grafts can be transplanted along with the muscle, skin, surrounding blood supply and innervation, which permits the simultaneous reproduction of both hard and soft tissue with satisfactory esthetic and functional results.1 The other donor sites suggested for reconstruction of the defective jaw are radius, scapula, thoracic rib, iliac crest, and fibula. It was Taylor et al who first reported the application of the vascularized free fibula flap.2 In 1989, Hidalgo et al modified the method for the restoration of partial mandibulectomy defects.3 Multiple case reports have also been depicted in the literature for the use of this graft to reconstruct an assortment of maxillary defects. Currently, the vascularized fibular graft is not only the best treatment modality for mandibular reconstruction but for the maxilla also. The documented advantages of the vascularized free flap fibula are:
Although reconstruction of defects using
vascularized free flap fibula is picking up
prominence with continued developments in its
techniques, it has a few difficulties. The substantial height difference between the reconstructed
mandible and the intact mandible can make
the prosthetic restoration of such patients very
demanding.7
Due to the reduced height of the
reconstructed mandible, a large vertical prosthetic
space is created from the crest to the occlusal
plane. If the crown-root ratio is greater than 1:1,
high leverage forces are created, which can be
detrimental to the implants in cases of exclusively
implant-borne super-structures, and to the
supporting teeth in free-end circumstances. This
can jeopardize the life span of the superstructure.
Additionally, deviation of the residual mandibular
segment toward the side of the defect results in
an abnormal maxillo mandibular relationship
and limited masticatory function.4
There are few available methods for compensating
the increased vertical height such as double barrel
technique for placement of fibula bone graft,
vertical distraction osteogenesis of the fibula,
placement of the graft 1cm higher than the lower
border of the intact mandible and prosthetic
management of the vertical height. These
surgical modalities are technique sensitive and
time consuming. Moreover, there is little literature
describing the various prosthetic options available
to decrease the crown height space and thereby
increase the longevity of the graft as well as the
implant placed. This paper aims at presenting
the prosthetic possibilities of management of
the increased crown height space with implant
supported prosthesis.
Patient 1
A 35 years old male reported to the Department
of Head and Neck surgery in 2013 with the chief
complaint of swelling in lower right mandible for 5
years. The clinical examination and investigations
confirmed the diagnosis as ameloblastoma.
Surgical resection of the lesion (segmental
mandibulectomy) and reconstruction of the region spanning lower right canine to molar was done
with free fibula flap under general anesthesia.
After a period of one year, a radiograph was
taken to ensure adequate union of the graft with
the mandible (Fig 1). Debulking of soft tissues
was done. Dental implant placement was then planned, where 3 dental implants of dimensions
3.7X11.5mm, 3.7X10mm and 3.7X13mm(Zimmer
Dental Inc., Carlsbad, Calif) (Tapered Screw
Vent®), in regions from first premolar to second
molar was carried out (Fig 2 and 3). After 5 months of
adequate osseointegration of implants, prosthetic rehabilitation in terms of a fixed hybrid prosthesis
was planned. Split thickness graft placement and
soft tissue debulking were performed to increase
the sulcus around the bone and the implant (Fig 4)

In the prosthetic phase, transfer copings were
attached to the implants and an impression was
made using closed tray transfer method with
addition silicone impression material (AQUASIL
soft putty, Dentsply, India) (Fig 5). Following this
maxilla-mandibular relation was recorded and
a wax trial was done for the interim prosthesis
(Fig 6, 7 and 8). After metal try in, the final hybrid
prosthesis with metal substructure and acrylic
wraparound was screwed onto the implants. (Fig
9 and 10)
The patient is followed up annually. Recently, in
May 2018 the patient reported with a complaint
of loosening of the prosthesis. On examination a
fracture of the connecting screw in relation to the
distal most implant was noticed along with screw
loosening in the anterior two implants. This may
have resulted due to the prosthetic design selected
for the excessive prosthetic space that existed.
(fig 11 and 12)
Patient 2
A 25-year-old female patient reported to the
Department of Head and Neck surgery in 2016 with
complaint of pain in right lower jaw and inability
to open mouth. Clinical examination revealed a tender swelling over the right mandibular ramus.
Radiographic and histopathological findings
confirmed the lesion as Odontogenic keratocyst.
The patient did not have any systemic disease and
all routine investigations were normal.
Management:
Mandibular resection was done followed by
reconstruction with free fibula flap under general
anesthesia (Fig 13). After a period of 5 months,
radiographic assessment was done. It showed
adequate integration of the fibula flap with
mandible. Implant supported fixed prosthetic
rehabilitation of right mandible spanning canine
to second molar region was planned. Impressions
were made and jaw relations were recorded.
Prosthetic space was assessed. Crown height space was found to be 17mm in the canine region
and 18 mm in the premolar region. A radiographic
acrylic stent was fabricated to determine the
implant position. (fig 14 and 15) A cone beam
CT was made. After taking into consideration
the crown height space and the buccolingual
relationship of the fibular graft to the opposing
teeth it was decided to go ahead with a prosthetic
rehabilitation using a hybrid denture with a milled
bar and acrylic wrap around.
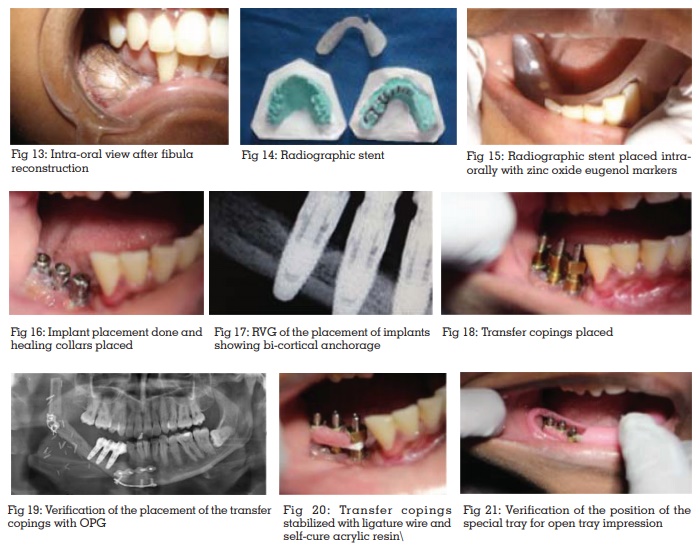
De-bulking of tissues was done prior to implant
placement. 3 dental implants (Nobel BioCare
Replace select® System, Zurich, Switzerland)
of dimensions 4.3x13mm in relation to canine,
4.3x10mm in relation to 1st premolar and 1st
molar were placed in the reconstructed mandible.
(fig16 and 17) After 3 months of healing and osseointegration, prosthetic rehabilitation was
done. An implant supported fixed hybrid prosthesis
was planned due to the amount of inter-arch space
available
Implant level impression was made with polyvinyl
silicone impression material (AQUASIL soft putty,
Dentsply, India), using customized open acrylic
resin trays. The transfer copings were stabilized
with ligature wire and pattern resin prior to
impression making. The impression was poured
with type IV dental stone to fabricate the definitive
cast. (fig 18 – 23)
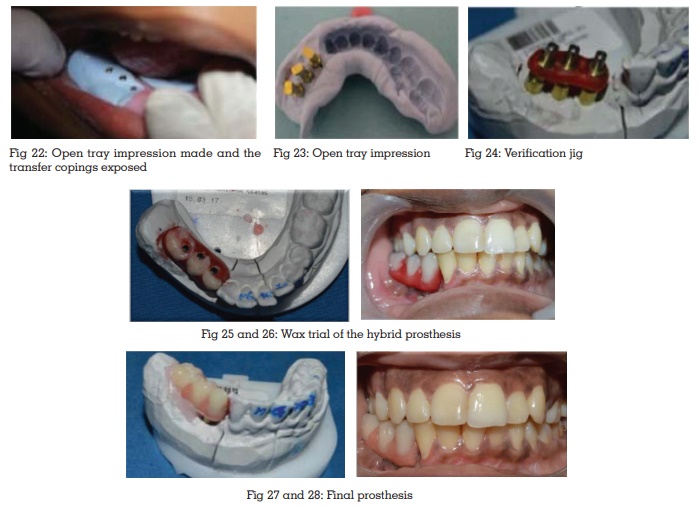
A jig trial was done to check the proper position of the abutments (Fig 24). A panoramic radiograph
was taken to confirm this. Thereafter, a wax try-in
was carried out (Fig 25 and 26). The final prosthesis
comprising a metal framework and an acrylic wrap
around with 2 premolars and a single molar was
screwed into position. (fig 27 and 28)
Patient 3
A 63 years old female patient reported to the
Department of Head and Neck surgery in 2016
seeking management for ameloblastoma that
was diagnosed elsewhere. Further investigations
revealed bony hard swelling clinically and a cystic swelling with lingual expansion radiographically
on left side of mandible, which confirmed the
diagnosis. With all blood investigations normal,
she was posted for surgery.
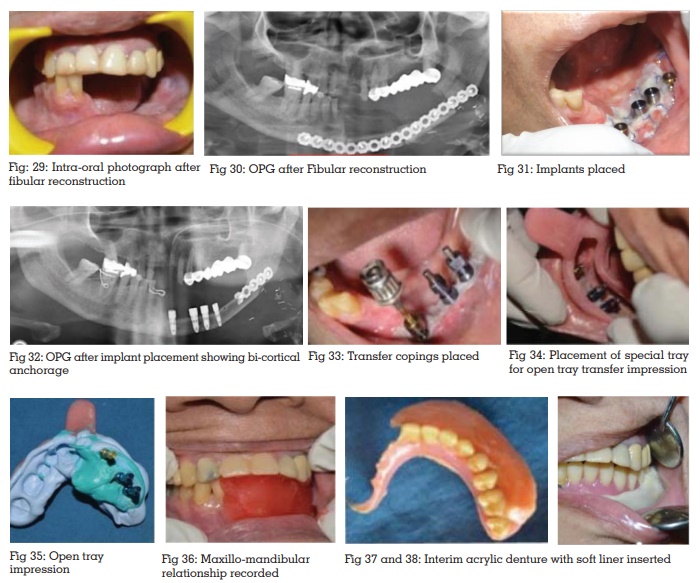
Management:
A left segmental mandibulectomy followed by
reconstruction with free flap fibula was performed
under GA (Fig 29). Radiographic assessment was
done after one year which showed a adequate
union of the fibula graft with mandible. (Fig
30) Impressions were made, jaw relations were
recorded. Prosthetic space was measured in the
cast it was found to be 23mm in the canine region
and 25mm in the posterior region. Owing to an
increased prosthetic space, it was decide to go
ahead with a Paris bar supporting an hybrid
denture retained with locator abutments. A second
surgery was done under general anesthesia where
vestibuloplasty and dental implant placement in
relation to 31, 33, 35 and 36 regions were carried
out. 4 Implants of dimensions 4.3X10mm (2) and 5X10mm (2) (Nobel Biocare Replace Select®,
Zurich, Switzerland). (fig 31 and 32)
After 6 months, panaromic radiograph was taken
to assess the dental implants. One implant failed
to integrate. Prosthetic rehabilitation was then
planned with CAD/CAM milled bar retained implant
overdenture to compensate for the increased inter-arch space. Implant level impression was made
using open tray transfer method with addition
silicone impression material. Transfer copings
were attached to the implants and secured with
orthodontic wires and pattern resin (Fig 33-35). A
definitive cast was fabricated with the impression
made. Maxillo-mandibular relationship recording
was done and an interim removable partial denture
prosthesis with soft liner was inserted. (Fig 36-38)
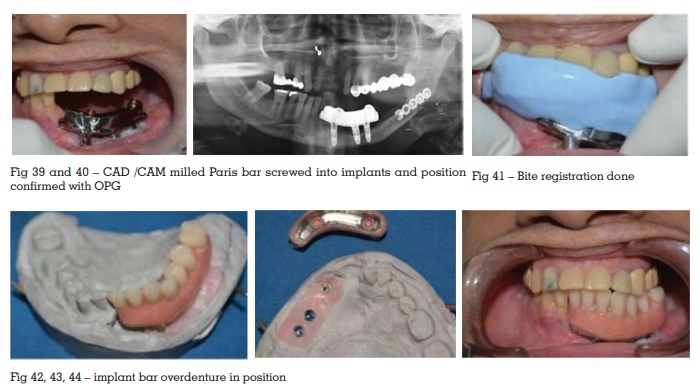
A CAD/CAM milled Paris bar (Nobel Biocare,
Procera, New Jersey, USA) was fabricated and
screwed into position. A panaromic radiograph
was taken to check proper seating of the bar into
the implants. (fig 39 and 40) Jaw relations were
recorded. (fig 41) The removable supra-structure comprising of
a metal framework with overlying acrylic resin
replacing the lower left dentition from central
incisor to first molar was inserted. (fig 42-44)
The patient continues to use the prosthesis till date
without any complications.
Reconstruction of severe maxillary and mandibular
defects to restore form and function continues
to be a challenge. Since being introduced in
1989 by Hidalgo, vascularized free flap fibula
has been the long-standing mode of treatment
of these defects. It is established that mandible
withstands high amounts of load and thus it must
be sturdy. This being said, fibula, being a tubular
bone with a thick layer of cortex, is considered to
be the sturdiest of all the vascularized grafts as
portrayed in the literature. Thus it is suitable for
withstanding the loaded intraosseous implants.8
Following reconstruction of the defects, prosthetic
rehabilitation is necessary for the restoration of
form and function. The design of the prosthesis
is based on the amount of crown height space
available and fulfillment of prosthodontic criteria
of support, stability, and retention.5
The various
methods in which prosthetic rehabilitation can
be carried out are using removable prosthesis,
implant retained overdentures, conventional
implant supported prosthesis, hybrid dentures
or implant supported bar overdenture.
Using removable prosthesis may create forces
on the underlying bone, opposing dentition and
the surrounding musculature.6
According to the
literature available, implant supported prosthesis
have an excellent long-term survival and success
rate (ranging from 86-99%) for implants placed in
reconstructed jaws.7-9 Hidalgo and coworkers have
reported a success rate of 100% for a series of 19
patients over a 10-year follow- up.3
Kramer reported
a success rate of 96.1% after an observation
period of 1400 day.7
Therefore, implant supported prosthesis is the preferred treatment modality.
Patient who have undergone reconstruction using
fibular graft present with an increased prosthetic
space. The buccolingual position of the fibula
may also not be favorable owing to the anatomic
differences in the contour of mandible and fibula.
the prosthetic design is dependent on the available
space and the position of the implants in the fibula.
When the prosthetic space is more than 15mm
a hybrid denture with an acrylic wrap-around
a milled bar is the preferred choice. When the
prosthetic space is in excess a hybrid denture can
impose cantilever load on the implants, resulting
in screw loosening or screw fracture When the
prosthetic space is in excess of 18mm a Paris bar
or similar substructures may be planned over
which a hybrid denture maybe retained using a
precision attachment. Figures 1- 12 show pictures
of a patient who reported with a failed prosthesis
with a fractured screw due to increased crown
height space, and improper prosthesis design.
Patient also reported difficulty in maintaining
oral hygiene.
A hybrid denture consists of a metal substructure
with an acrylic wrap around. Studies suggest
that there is an impact force generated during
mastication which is well tolerated by the resiliency
of the periodontal ligament fibers in natural
dentition, but in cases of implant supported
prosthesis, the impact of the force is tolerated by
the flexibility of the implant bone anchorage.11 It
has been hypothesized that a soft layer on the
prosthesis such as plastic or acrylic resin may
reduce the impact forces on the implant bone
interface.10 Consequently, a metal substructure is
used with an acrylic wrap-around. The treatment
of edentulous or partially edentulous patients with
hybrid dentures has been seen to accomplish more
noteworthy masticatory work and psychological
satisfaction than with regular over-dentures.
Additionally, use of screw-retained prosthesis is recommended for patients suffering from weak
denture retention because this type of prosthesis
can be easily placed and retrieved.4
Apart from
the said advantages, hybrid prostheses can also
replace soft tissue defects. It should be kept in
mind that passive fit is the prerequisite for survival
of implants in bone and not achieving it leads to
mechanical and biological failures. Passive fit can
usually be achieved through precise laboratory
work and special attention during framework.
The amount of inter-arch space decides the
use of hybrid prosthesis. For space of 15mm or
more, a hybrid denture can be recommended.
This restoration design uses a smaller metal
framework, with denture teeth and acrylic to join
these elements together. It is less expensive to
fabricate and is highly esthetic.12
An implant bar overdenture is typically a three-segment structure containing the embed, over
which a milled bar is put which acts a substructure
for a removable acrylic prosthesis with precison
attachments. This being said, it can be thought
to be a fixed removable kind of prosthesis. As
per M. Marinbach, there are two considerations
for prosthetic height. The first is the distance
between the connection framework to the crest
of the bone. The higher the crown height distance,
the more the stress connected to the bar, screws,
and implants. The second consideration is the
separation from the connection to the occlusal
plane This crown height represents the increase
in prosthetic stress applied to the attachment.
These conditions create a higher lever activity to
the prosthesis than at the implant interface and
results in increased instability of the restoration
during lateral forces. In such situations where
there is an increased crown height space, a hybrid
denture or an implant supported overdenture
will act as a vertical cantilever, amplifying off-axial load at the implant abutment interface.
There is also an increased possibility of tissue proliferation because of collection of debris. In
addition, in a fibula reconstructed mandible, the
implant abutment interface lies at a level lower
than whatever is left of the dentition, because of
the distance from the fibula. in order to discredit
the impacts of the torsional stress on the implant,
and diminish the vertical cantilever, a milled metal
sub-structure can be manufactured. This also
empowers uniform dissemination of forces in the
implant. A removable acrylic prosthesis can be
manufactured over this substructure with precision
attachments. This leaves an exceptionally polished
milled bar for the patient to maintain. There are a
few points of interest to such a prosthesis. The close
adaptation of the secondary casting to the milled
bar gives additional stability and retention which
is not accessible in implant supported prosthesis
as well as tissue-supported prostheses. The
inflexibility of the prosthesis braces the implants
by splinting them together. Moreover, it is negligibly
cantilevered (or lacks cantilevering), which brings
about a favorable biomechanical design. Sufficient
phonetics and esthetics are accomplished because
of the capacity to legitimately frame palatal
and labial shapes in the flexible compound.
Appropriate oral cleanliness strategies can be
performed by patients, and negligible soft tissue
coverage by the sub-structure promotes mucosal
health.
Excellent form and function can be achieved while using vascularized free flap fibula for the reconstruction of mandibular defects. In order to successfully rehabilitate reconstructed jaws, certain factors must be considered
CAD/CAM : Computer aided designing/ Computer
aided machining
The authors acknowledge the support received
from Head and Neck department and Department
of Prosthodontics, Amrita Institute of Medical
Sciences, Kochi. Authors are grateful to Dr Anil
Mathew, Professor and Head, and Mr. Vinod P
Nair, Chief technician, Amrita School of dentistry
for their unwavering support.
We know of no conflicts of interest associated with
this publication, and there has been no significant
financial support for this work that could have
influenced its outcome.