Context & aim: Precision attachments have the
potential to significantly enhance the performance
of our prosthetic treatment and render it
aesthetically pleasing. The aim of this survey is
to evaluate the awareness, knowledge and attitude
of dental practitioners (as the primary objective), &
lab technicians (as secondary objective) towards
precision attachments.
Settings and Design: A questionnaire-based survey.
Methods and Material: A survey with fifteen &
ten questions were prepared and validated to
analyse the awareness, knowledge and attitude of
dental practitioners and lab technicians towards
precision attachments respectively. The survey
was conducted via Google Forms.
Statistical analysis used: The data was analysed
based on qualification and years of experience
for the dentist-based survey and based on years
of experience for the lab technician-based survey
using Chi-Square test.
Results: The results of this survey show that
dental practitioners are aware of the importance
of precision attachments and their grasp of
treatment planning protocols also seems to be adequate. However, they are not confident enough to
independently handle cases of precision attachments
since they seem to be lacking in their fundamental
principles and scientific knowledge. Moreover, the
lab technicians included in the survey also stated
that lack of knowledge and skill of the practitioners
is the primary hurdle to a more optimum use of
precision attachments.
Conclusions: The use of precision attachments
presents a challenge in the current dental scenario
primarily due to deficiencies in treatment planning,
knowledge and technical skill.
Key words: awareness, knowledge, attitude, precision attachments, dental practitioners, lab technicians.
Precision attachments have been in use since a
very long time. Evidence of its earliest use dates
back to the Egyptian times in the 4th and 5th
century BC. However, development of precision
attachments as we know of today began only in
the early 20th century with Dr Herman E Chayes.
Precision attachments can offer considerable
benefits in prosthetic dentistry by enhancing retention, aesthetics, stress distribution and cross
arch stabilization.1
They can be used in a variety
of cases such as with removable prosthesis, fixed
dental prosthesis, implant supported prosthesis,
overdentures, maxillofacial prosthesis etc making
them extremely versatile.2-4 There are numerous
types of attachments currently available in the
market today and they can be broadly classified
based on location (intracoronalorextracoronal);
type (stud, bar, magnets and auxillary groups); and fit (rigid or resilient).5-10
The principal aspects to be considered in designing
cases of precision attachments are thorough
diagnosis, space analysis, comprehensive
evaluation of condition and location of abutment
teeth, precise establishment of path of insertion,
meticulous selection & position of attachments,
understanding patient compliance & their manual
dexterity and maintenance protocol to name a
few.11,12 These factors are extremely critical to
the success of the prostheses and must be
judiciously planned and evaluated.
A thorough understanding of the
different attachments, material science
& biomechanics of maxillomandibular
function are a fundamental prerequisite
in successfully treating a case with
precision attachments.1
A well planned
and executed prosthesis, coupled with
optimum maintenance and care, has
the potential of providing a robust
and enduring patient experience for
a long time. However, using precision
attachments involves a highly
technique-sensitive process. Even the
slightest miscalculation or violation
of biological and/or mechanical
principles at any step can result in
improper fit of the final prosthesis thus
making them highly tedious to use for
many practitioners.
Thus, the primary objective of this
survey is to evaluate the awareness,
knowledge and attitude of dental
practitioners towards precision
attachments and to assess if there
is a correlation of the above factors
with their qualification and years
of experience. For this purpose, the
sample has been classified into four
groups as per qualification (BDS,
MDS in Prosthodontics, MDS Others,
OTHERS i.e., DCI recognized diploma
and fellowship courses post-BDS ) and into three groups as per years of experience (0-10, 11-20
&>20 years).
Since lab technicians constitute an important link
in the successful use of precision attachments,
this survey also aims to evaluate the awareness,
knowledge and attitude of lab technicians towards
precision attachments based on their years of
experience (0-10, 11-20 &>20 years), as the
secondary objective.
A survey with 15 questions was prepared and
validated to analyse the awareness, knowledge
and attitude of prosthodontists and other dental
practitioners towards precision attachments (Fig 1).

Awareness of prosthodontists and other dental
practitioners was evaluated based on answers
obtained in question numbers 3,4,5,6,7,8,9.
Knowledge of prosthodontists and other
dental practitioners was evaluated based
on answers obtained in question numbers
10,11,12,13.
Attitude of prosthodontists and other
dental practitioners was evaluated based
on answers obtained in question number
14 i.e., the confidence to independently
handle cases of precision attachments.
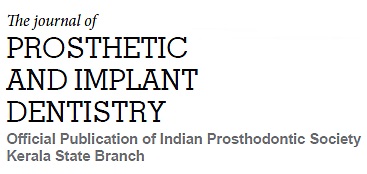
A survey with 10 questions was prepared
and validated to analyse the awareness,
knowledge and attitude of lab technicians
towards precision attachments (Fig 2).
This questionnaire-based survey was
conducted via google forms after prior
approval from the Institutional Ethics
Committee. Sample size was calculated
based on a pilot study conducted with
150 responses obtained from qualified
dentist (prosthodontists and other dental
practitioners) using the formula:
n=Z2pq/d2
n= Desired sample size
Z= Standard normal deviate (1.96)
p= Proportion in target population
estimated to have particular
characteristics (50% i.e. 0.5)
q= 1-p (Proportion in target population
not having particular characteristics)
d= degree of accuracy required (0.05)
Total sample size calculated was 384 for the
dentist-based survey; 391 responses were
included in this survey. Due to paucity of data
and resources, sample size was not calculated for
the lab technicians-based survey & 40 qualified lab
technicians were included. Convenient sampling
technique was used.
Dentists with BDS, MDS & DCI recognised diploma
courses post BDS degrees were included in the
dentist-based survey. Interns, Dentists with no-DCI recognised degrees and unqualified lab
technicians were excluded from this survey.
Data was collected as per responses obtained
via google forms, entered into Microsoft Excel
spreadsheet and was subjected to Chi- square
test using Statistical Package of Social Sciences
(SPSS) Software. This data was analysed based
on qualification (i.e. BDS, MDS in Prosthodontics,
MDS Others, OTHERS i.e., DCI recognized diploma
and fellowship courses post-BDS ) and years of experience (0-10, 11-20 &>20 years)for the dentist-based survey and based on years of experience
(0-10, 11-20 &>20 years) for the lab technician-based survey.
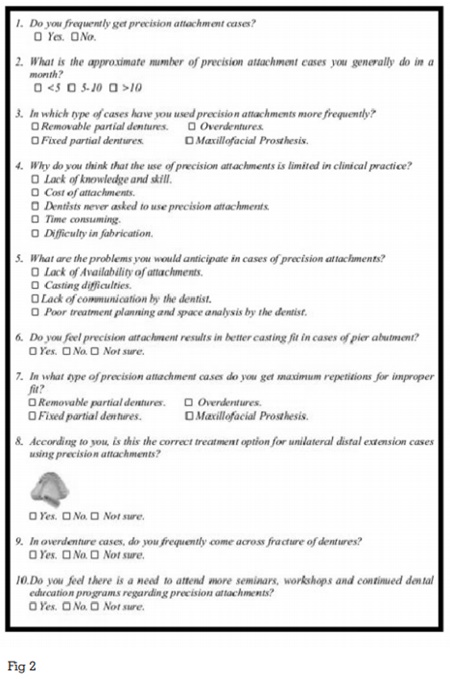
Dentist-Based Survey:
Out of 391 respondents,40% were BDS, 32% were
MDS in Prosthodontics, 25% were MDS in fields
other than Prosthodontics and 3% were from
Others category i.e., DCI recognized diploma
and fellowship courses post-BDS (Figure 3). Due
to unequal representation of ‘Others’ group, this
group was excluded from further evaluation to
avoid sampling bias.
Maximum positive responses for having used
precision attachments were elicited from ‘MDS in
Prosthodontics’ group in >20 years of experience
group. They primarily implemented precision attachments in Removable partial denture (54.1%)
> Overdentures (28.2%)>Fixed dental prosthesis
(16.5%) > 1.2% Maxillofacial Prosthesis cases
(1.2%).
Least positive responses were elicited from ‘BDS’
group in 0-10 years of experience group. This
limited use was attributed to lack of knowledge
and skill (51.9%) >Never felt the need (18.5%)
>Cost of attachments (9.3%) >Inadequate lab
support (8.3%) (Figure 4).
As mentioned earlier, awareness of prosthodontists
and other dental practitioners was evaluated
based on answers obtained in question numbers
3,4,5,6,7,8,9. Statistically significant results found in
questions 5 (P=0.012), 8 (P=0.023) & 9 (P=0.002).
Awareness was found to be maximum in ‘MDS
in Prosthodontics’ with 11-20 years of experience
group and least in ‘MDS others’ in 11-20 years of
experience group (Figure 5).
As mentioned earlier, knowledge of prosthodontists
and other dental practitioners was evaluated
based on answers obtained in question numbers
10,11,12,13. Statistically significant results
found in questions 10 (P=0.002) & 13 (P=0.009).
Knowledge was found to be maximum in ‘MDS in
Prosthodontics’ with 0-10 years of experience and
least in ‘MDS others’ in > 20 years of experience
group (Figure 6).
As mentioned earlier, attitude of prosthodontists
and other dental practitioners was evaluated based
the confidence to independently handle cases of precision attachments. Statistically significant
results found in question 14 (P=0.001). ‘MDS in
Prosthodontics’ with 11-20 years of experience seem
to have the maximum confidence to handle cases
of precision attachments. ‘BDS’ with 0-10 years
of experience group have the least confidence to
handle cases of precision attachment (Figure 7).
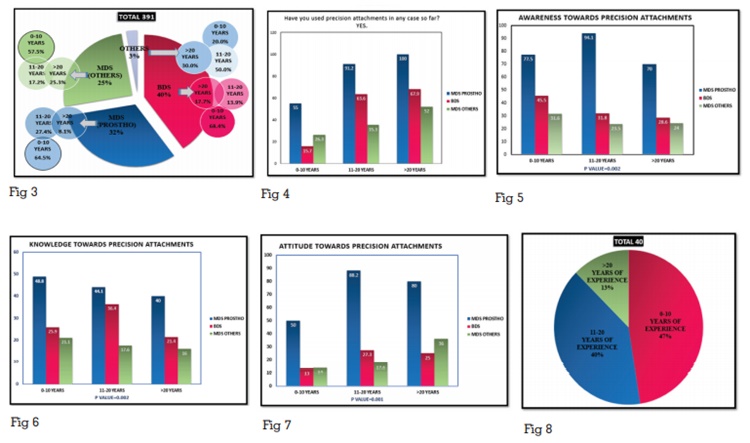
Lab-Technician Based Survey:
Out of 40 responses, 47.5% lab technicians had
0-10 years of experience, 40 % had 11-20 years of
experience & 12.5% had >20 years of experience
(Figure 8).
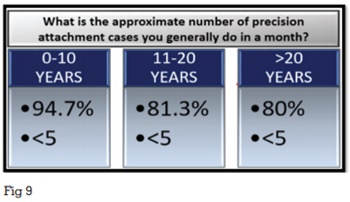
Statistically significant results found in the
questions 2 (P=0.05) & 4 (P=0.035). the results
showed that less than five precision attachments
are done per month by lab technicians in all the
groups of experience. This shows a general lack of
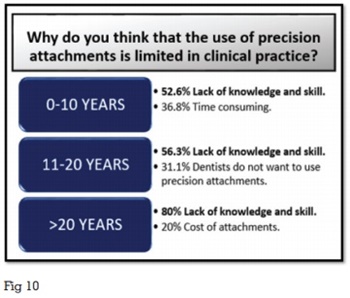
use of precision attachments (Figure 9). Also, lack
of knowledge and skill is the most common cause
for this lack of usage of precision attachments
(Figure 10).
This survey primarily aimed to find out about
the awareness, knowledge and attitude of
prosthodontists & other dental practitioners towards precision attachments. Under the awareness
subset, this survey evaluated the clinical mindset
and general approach of prosthodontists & other
dental practitioners during case selection towards
precision attachments. Under the knowledge
subset, this survey evaluated the theoretical
know how of prosthodontists & other dental
practitioners towards precision attachments. Under
the attitude subset, this survey mainly evaluated
the confidence levels of prosthodontists & other
dental practitioners to independently handle cases
of precision attachments.
The questionnaire was prepared after a detailed
search of published data available with respect
to precision attachments as well as inputs from
various practitioners.13-21
This survey shows that 72.1% of dental
practitioners are aware of the indications of
precision attachments and consider inter-arch space (80.6%), condition and location of
abutment teeth (85.2%) and manual dexterity of the
patient (66.8%) as important factors during case
selection.5,12,15 The practitioners do understand
the importance of precision attachments with
78% of practitioners accepting that precision
attachments could help provide better retention
in bilateral distal extension cases as compared
to conventional removable partial dentures and
50.6% of practitioners acknowledging that they
could get better results in pier abutment cases
using precision attachments.8,9,14 Their grasp
of treatment planning protocols seems to be
adequate with 73.1% practitioners being able to
correctly choose between tooth-supported and
implant-supported prosthesis based on individual
case requirements.6,21 Despite the above findings,
only 32.5% of practitioners are confident enough
to handle cases of precision attachments on their
own. Also, they seem to be lacking in fundamental
principles and scientific knowledge with only 31.1%
of practitioners being able to correctly differentiate
between precision and semi-precision attachments
and 35.8% of practitioners being able to correctly analyse the scientific basis of a certain prosthesis
design.
This survey also shows that knowledge about
precision attachments is maximum in ‘MDS in
Prosthodontics’ with 0-10 years of experience
group whereas awareness and confidence
to independently handle cases of precision
attachments is maximum in ‘MDS in Prosthodontics’
with 11-20 years of experience group. This can
be attributed to the considerable exposure to
precision attachment cases in their post-graduation
curriculum making young prosthodontists highly
knowledgeable in this topic. However, the clinical
know how and confidence develops with experience
and hence the middle-aged prosthodontists have
better awareness and confidence towards precision
attachments. This is in accordance with the result
showing that maximum positive responses for
having used precision attachments is from ‘MDS in
Prosthodontics’ group in >20 years of experience
group.
Least positive responses for use of precision
attachments were elicited from the ‘BDS’ with 0-10
years of experience group. This is in accordance
with the result showing that ‘BDS’ with 0-10 years
of experience group have the least confidence
to handle cases of precision attachment and the
reason for this limited use was stated to be lack
of knowledge and skill (51.9%). This is mainly due
to lack of exposure to precision attachments in
the BDS curriculum. This also explains their risk-aversion towards experimenting with precision
attachments.
Awareness is found to be least in ‘MDS others’
in 11-20 years of experience group. Knowledge
level is least in ‘MDS others’ in > 20 years of
experience group. Despite inadequate awareness
and knowledge, this group does use precision
attachments in their cases and the use is seen
to increase with years of experience as clearly
shown in figure 2. This is probably because of the
short courses and workshops available nowadays
enabling them to use precision attachments with increasing levels of confidence in their cases.
Only 32.5% of lab technicians stated that they
frequently received cases of precision attachments.
This clearly shows a limited use of precision
attachments in the dental set-up. Also, majority
of the cases they received were for removable
partial dentures (45%). When asked about the
problems they anticipated while fabricating such
prosthesis, they stated casting difficulties (50%),
followed by lack of communication(25%) and
poor treatment planning and space analysis done
by the dentist (22.5%). They also indicated that
they get maximum repetitions for improper fit in
fixed dental prosthesis cases (47.5%). 50% of lab
technicians felt that using precision attachment
results in better casting fit in cases of pier abutment
but 42.5% were not sure whether this improved fit
was purely because of precision attachments. Only
32.5% of lab technicians were able to correctly
identify a prosthesis design indicating a deficiency
of understanding the fundamental principles and
scientific knowledge.
This survey also found that 8.4% of respondents felt
that inadequate lab support was discouraging the
use of precision attachments in clinical practice.
However, the survey on lab technicians indicates
otherwise. As shown in figure 9, this survey found
that less than 5 cases of precision attachments
are being done per month by majority of the
lab technicians in all the 3 ‘years of experience’
categories. This clearly shows a general disinterest
for using precision attachments by the practitioners
since the number of cases do not seem to vary with
the ‘years of experience’ of the lab technicians.
This survey also clearly shows, that a majority of
the lab technicians feel that lack of knowledge
and skill of the practitioners is the primary hurdle
to a more optimum use of precision attachments.
The limitations of this survey include the small
sample size for the lab-technician based survey
and hence limited statistically significant results
were obtained for the same. Further questionnaire based surveys should be planned with a larger
sample size owing to the paucity of literature on
this subject.
The following conclusions were drawn based on the results of this survey: