Background: Implants splinted to natural teeth is
one of the treatment modality for the management
of partially edentulous patients. Even though lone
implant supported prosthesis is advocated, the
anatomical constraints may force the prosthodontists
to splint the implant to teeth. The advantages
of implants splinted to natural teeth includes
increased mechanoreception and additional
support for the force distribution throughout the
dentition. It also reduces the cost for the teeth to be
replaced and it avoids the use of cantilevers. But
Combining implants and teeth creates a potential
biomechanical mismatch of the supporting units as
both display different patterns of mobility under the
same physiological stresses. Hence the long-term
prognosis of this treatment method is a matter of
debate in dental literature. Other problems includes
marginal bone loss and various complications like
intrusion of the teeth, caries, mechanical failure, loss
of occlusal contacts have been reported associated
with this treatment approach.
Methods: A Medline search was conducted with the
key words :Tooth implant supported prosthesis, Tooth
implant connection, Stress distribution, Loading
condition, Tooth intrusion, Prosthesis design,
biomechanics. The research question was fabricated
according to PICO criteria: Can an implant be
splinted to a natural tooth? Search was limited
to articles published in English from 2000 to 2019.
Among them 28 articles were selected for review.
Conclusion: This article answers the research
question by reviewing the various aspects of the
biological and technical complications along
with the long-term survival rates of tooth implant
supported fixed prosthesis.
Numerous prosthetic techniques can be used
for the rehabilitation of missing dentition.1
The
method of rehabilitation depends upon the number,
arrangement, and status of residual teeth (eg,
periodontal health, remaining tooth structure);
cost; patient desires; and adequacy of the bone
to support dental implants1,2. Implant connected to
teeth has been considered as an efficient treatment
modality. This treatment is considered when there
is an anatomic limitation of space for implants or
failure of an implant to osseointegrate2
.
The advantages of tooth implant supported
prosthesis includes splinting of a natural tooth
to an implant, increased mechanoreception,
and additional support for the total load on the
dentition. In addition, connecting teeth with implant
broadens treatment possibilities for the restorative
dentist, reduces the cost for teeth replacement,
and avoids the use of cantilevers1,2. But the main
problem which was believed that when implant
connected to tooth, implant would be subjected
to increased stresses because of difference in
their mobility patterns3
. Several studies reported
the marginal bone loss or failure of implant
to osseointegrate. Various complications like,
intrusion of the teeth, mechanical failure, caries
and loss of occlusal contacts have been reported
in the literature2
.
The purpose of this article was to review the
literature regarding the rationale, difference in
the biomechanical behavior of the implant and the natural teeth, nature of connection, potential
complications associated and guidelines to be
followed when connecting implants and natural
teeth.
A Medline search was conducted with the key
words: Tooth implant supported prosthesis, Tooth
implant connection, Stress distribution, Loading
condition, Tooth intrusion, Prosthesis design,
biomechanics. A research question was fabricated
according to PICO criteria: Can an implant be
splinted to a natural tooth? Search was limited
to articles published in English from 2000 to 2019.
Among them 28 articles were selected for review.
The inclusion criteria involved randomized clinical
trials, prospective and retrospective clinical studies,
in vitro studies, finite element analysis, reviews and
biomechanical studies. Information regarding the
survival rate, complication rate, incidence of tooth
intrusion and type of connector used was collected
from the clinical studies. Abstracts, opinion articles,
and questionnaire based studies were excluded
from the review process. Various aspects of the
biological and technical complications along
with the long-term survival rates of tooth implant
supported fixed prosthesis was retrieved from
the reviews.
The Rationale for using tooth-implant connection
can be summarized into five categories. They
include Financial constraints1
, to gain support
from either the tooth or implant4,5, cases where
bone augmentation and placement of implants
is not possible6
, to preserve a tooth with good
prognosis4,5, to provide stability to prevent the
rotational forces4,7 and for esthetic reasons4,5.
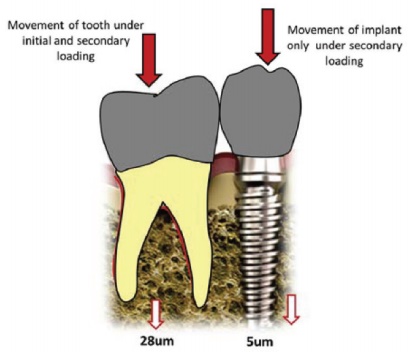
The natural teeth are attached to the alveolar bone
by means of periodontal ligament fibers; whereas osseointegrated implant is rigidly anchored to
the bone. This difference creates a potential
biomechanical mismatch of the supporting units2
.
The tooth exhibits normal physiological movement
in vertical, horizontal and rotational direction.
The primary factors influencing this movement
include the health of periodontium, number, length,
diameter, shape and position of the roots7
.
Due to lack of periodontal ligament, osseointegrated
implants exhibit linear movement during the entire
loading cycle without initial rapid movement.
This movement is because of the viscoelastic
nature of the bone7
. A healthy natural tooth can
move 200 µ in response to a 0.1 N force while
an implant can be displaced 10µ or less8
. The
ratio of the amount of movement of the tooth in
a healthy periodontium to that of an implant
has been estimated to be 10:1 and 100:19
. It was
suggested that physiologic movement of the
natural tooth causes the prosthesis to act as a
cantilever generating maximum resultant load up
to two times the applied load on the implant10,11.
Studies have also shown that teeth and implant
share the occlusal load and all the forces are not
transferred to the implant12,13. Resiliency of implant component,
cushioning effect of cement layer, and force
deflection in superstructure may contribute to
this phenomenon12–14. Therefore, biomechanical
impact of mismatching of mobility pattern
between the natural teeth and implant remains
controversial2
. When the applied load is concerned
both magnitude and duration of the force has
significant effect on the stress transferred to the
bone around a tooth. This may be significant in
patients with bruxism7
.
The advantages of splinting implant to tooth can
be summarized as follows:
Cavicchia reported that loosening and fracture of
fixation screws and abutments, ceramic fracture
and tooth migration seem to occur more frequently
in free standing implants compared to the tooth
connected restorations. This is due to the decrease
bite force in tooth-implant supported prosthesis
because of tooth related properioception16.
Despite of this, several studies indicated that
teeth in a TISP share the occlusal load and all the
forces are not transferred to the implant. Therefore,
various aspects of the data such as technical and
physiologic problems, theoretical concerns and
functionality of TISPs must be evaluated over a
time period to determine the benefits of connecting
teeth to implants12,13.
The disadvantages can be broadly classified into
technical and biologic problems5,17–19. The technical
problems mainly includes tooth intrusion, intrusion
of teeth with telescopic crowns, the Implant
fracture, cement bond breakdown, abutment screw
loosening, abutment tooth fracture, fracturing
of veneers and prosthesis fracture. The biologic
problems comprises of peri-implantitis, loss of
an abutment tooth, loss of an implant, caries,
endodontic problems, and root fracture.
Intrusion of the tooth is one of the most controversial
topics in the literature. Intrusion of the tooth in
TISP has been reported particularly with nonrigid
connectors or coping5
. When implants were
connected to natural teeth to support a fixed partial
denture, the incidence of tooth intrusion varied20.
Studies indicated that intrusion on an average
occurred in 3% to 5.2% of the cases4
.
An assessment was conducted by Reider and
Parel where they found that 50% of intrusions
happened in individuals with parafunctional
habits, specifically bruxism. They also noted that
it usually occurred in patients with nonrigid semi-precision attachments21. Many authors reported
that stress-breaking connectors were associated
with more intrusion than rigid connections1
. Some
authors discussed the causes of intrusion which
consists of:
Some authors reported that no intrusion of teeth
associated with rigid connectors17. Nickenig et al,
demonstrated that when rigid connectors were
used, results did not show any differences as if
restorations were screw- or cement-retained24.
Srinivasan et al has a contradictory opinion and
concluded that ‘the forces should be light, continues
and controlled to bring about intrusion without
damaging the tooth, in tooth-implant connection
it is not the case25.
The technical problems were related to the
preparation of abutment tooth, configurations
and dimensions of the bridge, cements employed,
opposing dentition, screws types, types of implants
and so on. Several studies reported more technical
problems associated with TISPs than ISPs. Naert
et al studied on 140 ISPs and 140 TISPs and
came to the conclusion that an ISP is more
preferable because of an increased number of
technical problems associated with a TISP. The
complication rate for a TISP was 5% to 10%(5).
Brägger et al reported that after 5 years, TISPs
did not have a higher risk of technical or biologic
complications compared with ISPs. However, after
10 years, TISPs had more failures than ISPs19.
Lang et al determined in their metaanalysis that
most of the technical complications associated
with TISPs occurred when there was a nonrigid
connection between abutment teeth. They also
concluded screw-retained restorations needed
more maintenance than cemented crowns17.
The amount of bone loss around abutments is
considered to be a critical determinant to evaluate
the durability of TISPs and ISPs. Isidor et al
reported that implant overloading can lead to
implant failure, which can progress to bone loss
at a later stage. It was also concluded with the animal studies which have shown occlusal load
may contribute to complete loss of osseointegration
or marginal bone loss26. Naert et al reported more
bone resorption around rigid than around nonrigid
connectors. However, the total additional bone
loss (0.7 mm) occurred over 15 years5
. According
to Albrektsson et al, amount of bone loss is within
the acceptable standards. This was based on a
criteria, which was <1.5-mm bone loss the first
year after implant insertion followed by <0.2-mm
per year in subsequent years27.
Hosny et al determined the amounts of marginal
bone loss around free standing and tooth-connected implants did not differ significantly.
They reported 1 mm of bone loss in the first 3 to 6
months after abutment connection and then 0.015
mm annually for 14 years(33). Bone levels around
the implants were found to be stable suggesting
that excessive loads did not occur to implant when
they were connected to teeth. Gunne et al and
Lindh et al also reported bone resorption around
implants incorporated in a TISP was similar to
bone loss adjacent to implants in an ISP when
assessed within the same individual15. In another
study, conducted by Block et al concluded that
there was no difference in the amount of bone loss
around implants that employed a rigid or nonrigid
connection. They noted that teeth around a rigid
connection was tend to have more bone loss8
.
CelsoHita-Carrillo has classified the methods
of connection into two main groups: Rigid and
nonrigid connection29.
Chee et al believe that rigid connection of the teeth
to the implants is not rational due to the adverse
effects on the implant in long-term. It will produce
greater marginal bone loss, with a corresponding
increase in probing depth around the supporting abutment27. Several studies suggest that the
tooth and bone implant components were able
to undergo some deformation to compensate for
the differences in the implant and tooth resiliency
under functional load28. Several authors concluded
that rigid connection achieves better outcomes
with regard to avoiding dental intrusion. Lin et al
conducted a Finite element anaysis and showed
greater stress concentrated on the neck of the
implant and the connector near the tooth29.
Intermobile elements: Some studies reported that
these elements provide flexibility to compensate for
the mobility of the tooth. An in vitro study conducted
by Chee et al, concluded that intermoblie elements
did not contribute to the flexibility of the system
and the bending force was transmitted to the
retaining screw of the implant abutment7
.
Attachments: Several studies demonstrated that
the attachments reduced the level of stresses in
the bone, because it breaks the stress transfer
process. It compensates for dissimilar mobility of
the tooth and Implant. But there were instances
of intrusion in 3 to 4% of the cases which lead to
cantilever formation on the implant increasing
the unfavorable stress formation on the implant
and the prosthesis30.
According to Hoffmann and Gregory, in 2012
reported that nonrigid connections drastically
reduce the stress on the superstructure while
increasing the forces on the supporting teeth and
implants3.
Hosny et al compared different combinations of
abutment teeth: single tooth and single implant,
multiple teeth connected to an implant, and
multiple implants connected to a tooth and reported
that no prostheses demonstrated adverse results.
The cases were monitored for 1 to 14 years. No implants were lost, and no differences in marginal
bone loss were observed between the treatment
groups28. Lindh et al conducted a 2-year follow-up
of various maxillary prostheses. One side received
an ISP and the other a TISP. Author concluded
that there was no difference in the failure rate
of implants (88% cumulative survival rate) with
different prosthetic designs and no bone loss was
seen with the TISP(30). Naert et al also monitored
patients with TISPs and ISPs. It was found that the
cumulative success rates of the implants for TISPs
and ISPs were 95% and 98.5% respectively. No
significant differences was observed with regard
to loss of implants even though the implants lost
were more with TISP. With regard to the cumulative
success rate of the prostheses, no statistically
significant differences between ISP (98.4 %) vs
TISP (94.9%) were noted5
.
The following guidelines (by Greeinstein et al)
which can prevent intrusion of teeth and enhance
patient care when contemplating fabricating a
TISP can be considered1:
Connecting implant to tooth was found to be a
controversial topic with literature showing both
success and failure rates for this condition.
Only limited long term clinical studies exist to
substantiate the results. No conclusive studies
were available to show the best prosthesis span
length which can be supported by connecting
implants to teeth. Despite the non rigid connectors
showing a more favourable force distribution, rigid
connectors achieve achieve better outcomes with
respect to long term stability, complications and
tooth intrusion. Though the incidence of marginal
bone loss around implants is still greater. Various
guidelines have been suggested by different
authors which aim toward increasing success
for such type of prosthesis. The risk and benefits
should be thoroughly analysed for each scenario.
Further research is still required for improvement
in the design pattern for facilitating usage of such
implant connected to tooth systems.