The extraction of teeth is inevitability associated with distinctive changes in the surrounding hard and soft tissues. The alteration of ridge contour may compromise the position of implant which requires optimal support and stability. To facilitate bone regeneration The Ice Cream Cone Technique” was introduced. It uses a collagen membrane in the form of an ice cream cone and bone filler material placed into it, to regenerate the buccal plate of a fresh socket without elevating a flap. This ice cream cone technique help to overcome the dilemmas which could otherwise result in loss of bone graft materials, gingival tissue collapse and invasion of graft by connective tissue.
Reabsorption of alveolar process occurs after the
dental extraction. The form of the tooth, their axis
of eruption and eventual inclination determines the
shape and volume of the alveolar process7
. Due to loss of bundle bone and the nutrient supply by
the periodontal ligament there will be bone loss in
the lingual and buccal plate of a post extraction
socket.
The vertical and horizontal bone loss cause aesthetic defect in the anterior zone. So it is
important to perform correct extraction technique.
For that atraumatic technique is performed using
traditional methods, specialized extractors,
periotomes and endodontic files or piezo surgery
for the removal of radicular elements8.
Buccal wall socket defect or loss can be due
to many factors with a common factor being
periodontal lesion Periodontal lesions can cause
bone resorption and destruction during lesion
expansion, leading to sinus discharge or chronic
swelling6. Socket collapse will occur after the
extraction of a tooth with periodontal lesion, which
will lead to fibrous tissue formation and narrowing
of the alveolar ridge.
Tarrnow, invented his technique (ice cream cone)
to augment the socket with buccal dehiscence,
but his technique is only recommended for simple
dehiscence and not a wall defect. In this technique
it involves shaping the collagen membrane into
an ice cream cone shape and placing it inside
the extraction socket. It will cover the dehiscence
site and the socket occlusally at the same time.
This technique is not applicable for a completely
defective or missing bone wall unless a flap is
raised and a guided bone regeneration (GBR)
procedure is performed.
Elian et al, developed a post-extraction fresh socket
classification system2.
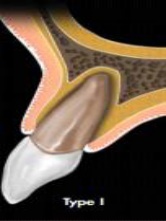
Type 1: The facial soft tissue and buccal plate of
bone are at normal levels in relation to the cement
enamel junction of the pre-extracted tooth and
remain intact post extraction.
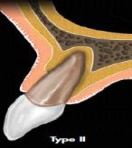
Type 2: Facial soft tissue is present but the buccal
plate is partially missing following extraction of
the tooth.
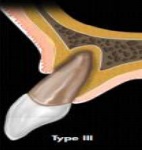
Type 3: The facial soft tissue and the buccal plate
of the bone are both markedly reduced after tooth
extraction
This classification enabled ordering and
classifying of post-extraction sockets. A recently
published sub-classification of type 2, now allows
even greater clarity to plan regeneration; type 2
presents intact facial soft tissue3.
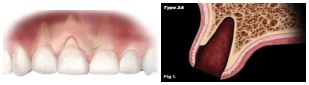
Type 2 A: Absence of the coronal one-third of labial
bone plate of the extraction socket 5mm to 6mm
from the free gingival margin.
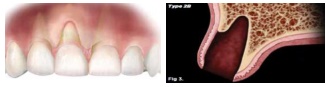
Type 2 B: Absence of the middle to coronal twothirds of the labial bone plate of the extraction
socket approximately 7mm to 9mm from the free
gingival margin.
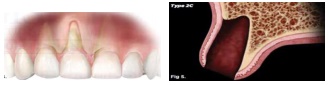
Type 2 C: Absence of the apical one-third of the
labial bone plate of the extraction socket 10 mm
or more from the free gingival margin
With the evolution of socket preservation and
socket grafting, many grafting materials and
techniques have been reported. Many reports
agree that socket grafting preserves the socket
collapse and it is better than a non-grafted socket
or a socket that underwent normal healing. Other
studies have found that covering the grafted socket
with a collagen membrane or soft tissue graft provided better results than uncovered grafted
or non-grafted sockets in terms of the amount of
bone formation6.
One reason for this result is that the collagen
membrane preserves the blood clot, maintains
the space and prevents soft tissue migration into
the socket.
However, using bone graft material alone without
a collagen membrane or soft tissue coverage may
result in a lower percentage of bone formation
A study conducted by Bozidar et al. showed
that sites that were grafted with a membrane
demonstrated a more uniform bone structure in
both the apical and coronal regions of the sockets6.
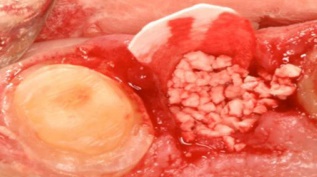
STEP 1
Once the tooth is diagnosed as hopeless, it is
removed atraumatically, it is performed utilizing
flapless extraction with care not to disturb the
interproximal papillae and labial soft tissue.

STEP 2
Socket is debrided with surgical curettte and any
infected tissues is removed.
A finger should be placed over the buccal tissue
when curetting the buccal part of the socket to
prevent perforation of soft tissue
STEP 3
A collagen membrane is contoured into a modified
V shape/ice cream cone shape. The narrow part
of the membrane is placed into the socket and
wide enough to extend laterally. Wider part of
the membrane should be trimmed and be able
to cover the opening of the socket.

STEP 4
The socket is then filled with a bone graft and the
pressure from the graft against the membrane will
help to keep it in place.
STEP 5
The top part of the membrane is extended over
the opening of the socket.

STEP 6
The membrane is then sutured with two or three
absorbable sutures to the palatal tissue.

STEP 7
It is then finished with a continuous suture.

This is an minimally invasive socket repair
technique which resulted in smaller contour
changes compared with flap elevation and
nontreated extraction sites with type 2 sockets.
This technique offers repair with less soft tissue
manipulation while allowing for secondary wound
healing5.