One of the core tenets of dentistry is prosthetic dentistry. Preventing the factors that lead to tooth extractions may be the most successful prosthetic prophylaxis. Modern treatment options significantly improve the quality of life for affected patients as well as the overall prognosis of the stomatognathic system. The importance of any procedure that can delay or eliminate future prosthodontic problems has been highlighted by preventive prosthodontics. The current review was carried out after conducting a thorough literature search across peer-reviewed publications and gathering data on preventive prosthodontics. The present article addresses the idea of preventive prosthodontics, encompassing the primary, secondary, and tertiary stages of prevention. The prosthetic interventions and procedures that can be performed at each stage are discussed.
Key words: preventive prosthodontics, denture, implant, root submergence
The growing population of elderly people has
not only increased their medical needs but also
their dental needs.1 One of the essential pillars of dentistry is prosthetic dentistry. The principal
aim of prosthetic dentistry is to follow the golden
statement by MM Devan (1952), “Perpetual
preservation of what remains is more important
than the meticulous replacement of what is
missing”.2 It is a universally accepted fact that
prevention is better than cure and Preventive
Prosthodontics signifies the importance of any
procedure that can delay or eliminate future
prosthodontic problems.3
Goals of Preventive Prosthodontics4
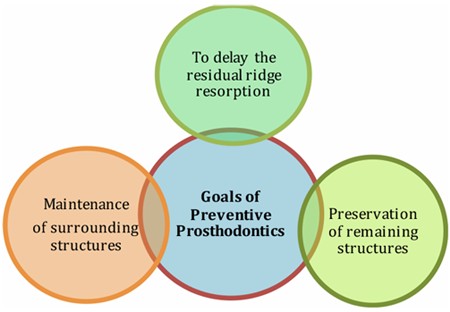
Preventive prosthodontics emphasizes the
preservation of existing oral structures while
minimizing the need for extensive future
restorations and timely prosthetic interventions.
It promotes a holistic, patient-centered approach,
ensuring functionality, esthetics and sustained
oral well-being. It can be studied under the
following strategies:
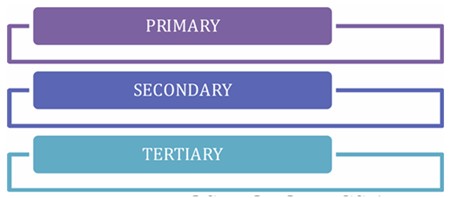
Preventive Prosthodontics At Primary Level
Prenatal Stage
It begins with prenatal care and clinical
assessment. A thorough guideline of nutritional
requirements during pregnancy and lactation is
essential, followed by prenatal fluoride therapy,
prevention of certain antibiotics that may harm
the dento-facial growth, and reinforcing oral
health care in pregnant women.
Postnatal Stage
Preventive prosthodontics at this stage focuses
on maintaining integrity of normal developing
dentition by including clinical assessment of
oral growth and development, pathology, and/or injuries, inclusion of anticipatory guidelines that
include home dental care.
Obturator
It is used to close a congenital or acquired
tissue opening primarily of the hard palate and
contiguous alveolar tissues. Immediate obturator
is placed immediately after the surgery with or
without surgical packing, it helps re-establishing
the oral contours, prevents the regurgitation
of the fluids in the nasopharynx, protects the
wounds from uneventful healing and prevents
the cicatrisation or shrinkage. Interim obturator
can be given after the removal of the surgical
packing. The interim obturator is retained up to
3 months with repeated checking and relining
with the tissue conditioner, followed by definitive
obturator.6
Adolescent Stage
Fluoride rinses and fluoridated toothpastes,
periodic scaling,
sealant
therapy
and
radiographic examination at regular intervals
are recommended. The primary prevention also
involves the protection of the dentoalveolar
structures from injuries such as tooth fractures,
concussion, crown root fractures, TMJ fractures,
dentoalveolar fractures, sport related and soft
tissue injuries with the use of mouth guards.7
Mouth Guards
Use of mouth guards reduced the risk of dental
and maxillofacial trauma less than 7.5%. The
mouth guards with moderate resiliency absorb
the forces, protect the teeth, TMJ and prevent the
contact of teeth and thus prevent ankylosis.8
Radiation Shields
Radiation shields / radioprotective stents are
used for the patients who are undergoing the
radiotherapy. The protection can be provided
by various methods like providing the radiation docking devices, making spacers in the
interstitial brachytherapy for tongue cancer and
fabrication of tongue shields.9
Preventive Prosthodontics at Secondary Level
It includes the early detection of the disorders
and providing prompt treatment. Various
treatment modalities include preventive resin
restorations of initial caries, direct and indirect
pulp protection, scaling and curettage, etc.5
Preventive prosthodontic procedures which
can be performed at this level are occlusal
interference correction, treatment for bruxism,
treatment for trauma from occlusion (TFO),
correction of plunger cusps and treatment of
obstructive sleep apnea.3
Occlusal Interference
Occlusal interference is any tooth contact that
inhibits the remaining occluding surface from
achieving stable and harmonious contact. If
the occlusal interference cross the threshold of
adaptive capacity of the Temporomandibular
joint, muscles of mastication and neuromuscular
system, it leads to muscle hypertrophy, muscle
fatigue, spasm, headaches, craniomandibular
dysfunction syndrome, wear facets, fractured
cusps, tooth mobility, parafunctional habits like
bruxism. Hence correction of occlusal interference
is recommended in the early stages.10
Bruxism
Is a condition where the patient tries himself to
equilibrate the occlusion and thus develop the
habit of clenching or grinding of teeth. This can
occur due to periodontitis, over a contoured
restoration, psychological and physical stresses,
sleep disorder, CNS disturbances and alcohol.
Bruxism leads to attrition, mobility, muscle
hypertrophy, occlusal facets, alveolar bone
loss and TMJ disorders. Treatment of bruxism
involves controlling the psychological stress, occlusal correction, coronoplasty and occlusal
splints or intraoral orthoses.11
Trauma from Occlusion (TFO)
It is a reversible condition. Acute TFO is due
to sudden heavy forces. Chronic TFO is due to
continuous and long duration occlusal forces,
e.g. bruxism, drifting and extrusion of the teeth.
Primary TFO is caused due to high occlusal
forces whereas main cause of secondary TFO
is a low threshold or low resistance of the
periodontium. Occlusal corrections are needed
for the correction of the TFO.12
Plunger Cusps
The cusps which wedge the food forcefully into
the interdental spaces of the opposing arch.
These plunger cusps are usually the functional
cusp (i.e., palatal cusp of maxillary teeth and
buccal cusp of mandibular teeth) and sometimes
palatal incline of maxillary buccal cusp and
buccal incline of lingual cusp. Treatment
involves rounding and shortening of the plunger
cusps and the opposing interproximal space is
protected by splinting the adjacent teeth.12
Obstructive Sleep Apnea
It is characterized by cessation of airflow
through upper airway while diaphragm
movement continues. It can cause due to
enlarges tonsils, enlarged soft palate, large
tongue and retrognathism. This can be taken
care by fabrication of prosthetic mandibular
advancement appliances like soft palate lifters,
tongue retainers, mandibular repositioners,
snore guards etc., and surgery to remove portions
of the soft palate and uvula.13
Preventive Prosthodontics at Tertiary Level
Tertiary level prevention involves limiting the
disability of the patient and rehabilitation.
Prosthodontic rehabilitation incorporates procedures like post and core treatment,
removable dentures, fixed dental prostheses
and implants.14
Timing of Extraction
Planned extraction of highly mutilated teeth
prevents the rapid resorption of the alveolar
ridges. Careful extraction should be done to
avoid the presence of unantagonized tooth. If
antagonists are not present, supra eruption of
opposing dentition leads to contact between
the mucosa and teeth of the opposing arches.
As a result, arch stability is lost, and this leads
to severe resorption of the alveolar ridge in
edentulous arch.15
Interim Denture/Treatment Denture
In the case of early loss of the permanent teeth,
if the definitive treatment cannot be done for
various reasons, the interim denture (treatment
dentures) can be utilized as preventive
measures. The treatment dentures acts as space
maintainers, prevent the migration, prevent the
supra eruption and prevent the contact between
the teeth, alveolar ridge, restore the function,
esthetics, restore the muscular tonicity, restore
the vertical height, jaw health and avoids the
abnormal jaw habits.16
Provisional Restorations
After the tooth preparation is done for fixed
prosthesis, provisional restoration is advocated
to prevent the events like pulpal inflammation,
mesial migration, supra eruption and arch
integrity, protection of the tooth preparation
margins and protection of the periodontium.
Clinicians have many choices of provisional
materials from which to choose when fabricating
provisional restorations. While traditional
materials are still in use today, temporary
materials are continuously being updated and
improved upon.17
Single Complete Denture/Complete Denture
When the teeth are completely absent in any one
of the arches, the fabrication of a single complete
denture is recommended, to restore function,
vertical dimension, esthetics and prevent the
development of parafunctional habits. The
complete dentures are provided with various
occlusal schemes such as balanced occlusion,
lingualized occlusion, neutrocentric concept
and others depending upon the condition of the
patients.18
Tooth retained over dentures
Some authors advised to retain the stumps
beneath the artificial teeth, and stated that
these roots maintain the alveolar bone health
and height for longer duration. This can be
achieved by fabricating an overdenture. This
can be advantageous in terms of conserving the
natural teeth, reducing the rate of residual ridge
resorption, proprioceptive feedback by existing
periodontal ligaments and thus controlling
the occlusive forces and preventing the rapid
residual ridge resorption.19
The success of a future maxillofacial prosthesis
can be greatly enhanced by careful presurgical
evaluation and communication involving the
patient, the surgeon, and the prosthodontist. It is the responsibility of the prosthodontist to educate
surgeons about the prosthodontic requirements
for restoring the patients that undergo ablative
surgeries. The prosthodontist should suggest
the advantages of removing or retaining tissue
adjacent to the surgical site.
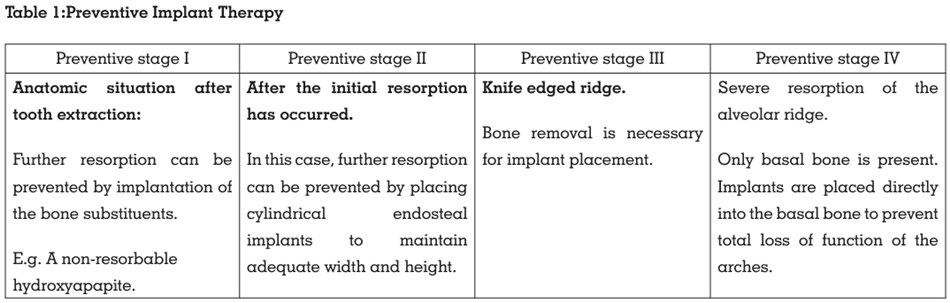
Preventive implantology is concerned with
the preservation of the alveolar ridge of the
(edentulous) jaw. Kalk et al. proposed the
resorption stages of the residual ridges which
are used in preventive implantology (Table 1).
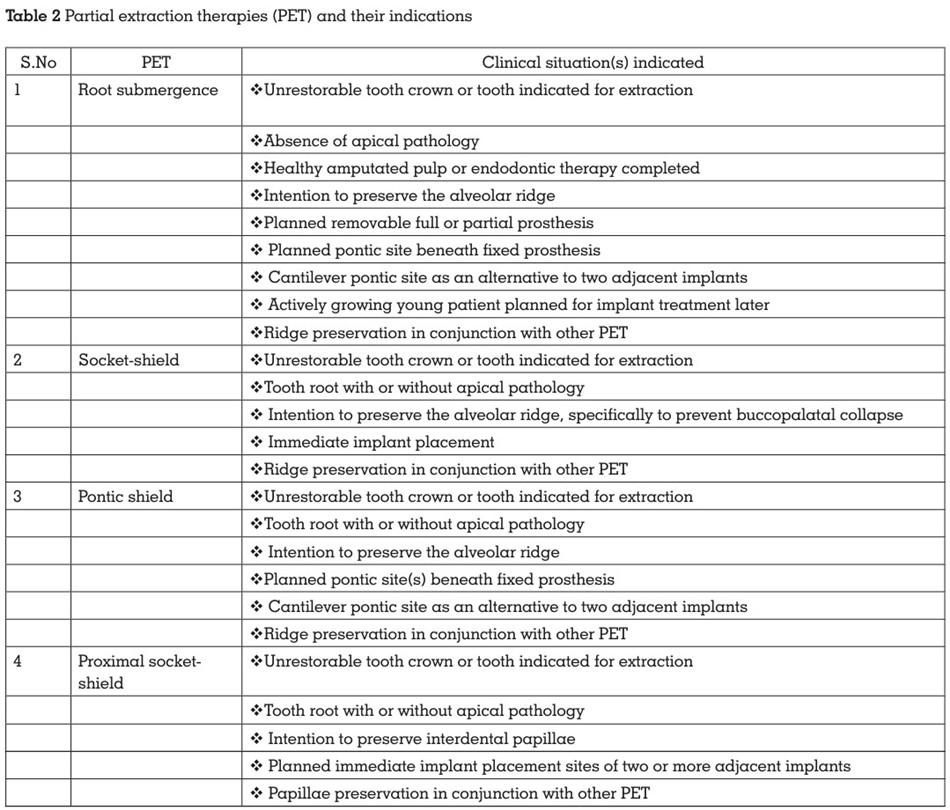
PET represents the collective use of tooth itself
to offset the loss of alveolar tissue (Table 2). By
retaining the tooth root and its attachment to
bone, the bundle bone-periodontal ligament
(BB-PDL) complex with its vascular supply may
be maintained. The techniques include
Prevention is both a dental profession’s
responsibility and an imperative obligation
to patients. Despite being a speciality area
for replacing lost teeth / soft and hard tissues,
prosthodontics cannot be disregarded for its
preventive value. A preventative prosthodontic
procedure can be carried out methodically to
address and prevent various issues.