PURPOSE- To calculate the marginal bone loss occurring around short and long implants placed
using bone condensing osteotomes as well as
using conventional drilling and to understand
the viability of osteotome technique and short
implants.
MATERIALS AND METHODS- An in‑vivo study
was undertaken to evaluate the crestal bone loss
on mesial and distal aspect of short and long
implants placed via osteotomes and conventional
drills (group A,B,C,D 5 implants per group) using
standardized intra‑oral periapical radiographs
at baseline,3 months and 3 months post loading
Statistical Analysis Used: Student’s unpaired t‑test.
RESULTS- Long implant via drills and osteotomes
were group A and B and their results were
statistically significant different (p < 0.004), short implant via drills and osteotomes were group C
and D where better bone level was observed for
short implant via osteotomes, when compared long
implant via osteotome (group B) and short implant
via osteotome The results show that bone level
measurement at 3 months post loading were higher
at mesial (0.52mm) and distal (1.06mm) positions for
long implants compared to short implants placed via
osteotome. The results were statistically significant
(p<0.05).
CONCLUSION- Considering the limitations of
implant placement in the posterior maxilla,
osteotome and short implants are a non-invasive
and predictable procedure for allowing implant
placement and bypassing the invasive surgical,
bone augmentation and graft procedures.
Key words: Atrophic maxilla, osteotomes, short implants, marginal bone loss, bone condensation
Endosteal dental implants are devices placed into the alveolar and/or basal bone of the maxilla or mandible that transect a cortical plate. They can be used to support and retain fixed dental prostheses, removable dental prostheses or maxillofacial prostheses.1 Quality of life in adults can be highly affected by tooth loss as a consequence of compromised oral function, loss of social status and diminished self-esteem.2 Prevention of atrophy after tooth extraction by socket or ridge preservation or reconstruction of the alveolar crest in cases of atrophy by augmentation with autologous bone or bone substitute materials of different origins have become reliable treatment options to establish a sufficient implantation bed. However, extensive augmentation procedures as therapy of choice for all patients should be viewed critically. Due to compromised general health, anamnestic data, or individual demands of the patient, minimally invasive methods to restore oral function should be considered.3 Conventionally surgeons aim for placement of the longest possible implant in any given site as long as the bone was available its placement does not hinder the final prosthetic result in terms of esthetics. This was especially crucial in the past, when implants presented a machined surface and the most common way to increase implant-to-bone contact was to increase the surface area available by placing a wider or longer implant. The longer and wider implants were clearly associated with higher success rates at that time when placed in similar intraoral sites. However, the posterior maxilla presents a uniquely challenging site for implant placement due to several complicating factors. Some of the factors that lead to difficulties in implant placement and success in the maxillary molar region are:
Different surgical techniques enabling the
reconstruction of maxillaries with reduced bone
height have been described in the literature. These
procedures allowed the implant rehabilitation
in situations that implant placement would be
contraindicated in the past. Several surgical
techniques have been advocated for vertical
bone augmentation of severely resorbed ridge,
such as guided bone regeneration combined
with bone graft, the interposition of bone block
grafts (inlay technique), sinus elevation, and
distraction osteogenesis. The inferior alveolar
nerve lateralization and transposition are the
examples of uncommon procedures in the
mandible. In this scenario, the placement of short
implants appears as an alternative treatment to
avoid advanced surgical procedures and their
corresponding morbidity.5
The posterior maxilla
is one of the most challenging anatomic locations
for the implant placement that requires adjunctive
surgical procedures. This special study covers
leading researches and reviews on this topic that
we believe would contribute to clinicians.6
In the last
ten years, the use of short implants has increased
significantly, especially in partially edentulous
maxillae but information regarding extra-short
implants (<7 mm) remains limited7
. Studies have
explored the short-term and long term survival
rates of short implants <6 mm). Unfortunately,
the evidence supporting the use of short implants
(<6 mm) in the posterior maxilla is weak, and no
guideline statement is currently recommended8
.
Implants <10 mm with traditional machined
surfaces showed inferior success rates compared
with longer implants in the past. So due to the sinus pneumatization placement of long implants
requires a sinus lift via a lateral window osteotomy
(LWO) but it does have some disadvantages,
including a higher cost, increased morbidity,
risk of serious infection, and delayed healing
time.9
As a less invasive alternative, osteotome.9
techniques can obtain a localized elevation of the
sinus floor through a 3-mm– to 6-mm–diameter
crestal osteotomy, which minimizes the degree
of flap elevation and thus eliminates the need for
preparation of a larger bony window in the lateral
aspect of the alveolus When there is adequate
subantral bone for the primary stabilization of
implants, osteotome-mediated sinus floor elevation
(OMSFE) procedures procure 2 mm to 7 mm of
localized sinus floor elevation, usually permitting
the simultaneous placement of implants of 10 mm
or lesser in length.10 The Osteotome technique
was first detailed in multiple publications by
Summers where use of blunt instruments called
Osteotome were used for elevation of the sinus,
bone augmentation occurs followed by dental
implant placement simultaneously or four to six
months later as a two-stage technique.11 This
made it possible to insert the Osteotome within
the maxillary bone and compress the latter –
there by affording increased bone density for
the preparation of beds of the same diameter
as the required implant. The placement of
implants in narrow maxillary crests in a single
surgical step, involving the use of expansion
osteotomes,has become a routine, predictable
and easy technique.12 So to highlight the technical
and biological complications associated with
both short implants, and compare the marginal
bone loss occurring around them when placed
via surgical Osteotome and conventional drills
the present study is being conducted.
Aim:
Objectives:
The present study was carried out in Department of
Prosthodontics, Vyas Dental College and Hospital,
Jodhpur from Nov 2019 to Dec 2021. This in vivo
study was performed after approval was received
from Institutional review of Vyas Dental College
& Hospital (11/2019).
A total of 24 implants were placed in patients
reporting to the out-patient Department of
Prosthodontics and Crown and Bridge and
Implantology, Vyas Dental College and Hospital,
Jodhpur based on the inclusion and the exclusion
criteria.
Study was divided into following groups based on the length and technique of placement
Detailed medical and dental history of each patient
was taken. After an explanation of the proposed
study criteria, including alternate treatment,
potential risks and benefits, the participants were asked to sign an informed consent.
After evaluating bone height from the crest to
the sinus floor, if that was greater than >5mm
long(>8mm) implant was planned for groups A
and B, placement was via drills for 5 subjects of
group A and via osteotomes for 5 subjects of group
B. If the residual bone height was less equal to 5
mm short implants (8mm) were planned for Groups
C and D, placement was via drills for 5 subjects
of group C and via osteotomes for 5 subjects of
group D. The implants used were ADIN TouaregTM-S
Spiral dental implant along with all the surgical
armamentarium. Required for placing implant.
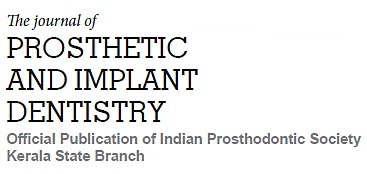
(Fig 1)
On the day of surgery the patient was prepared
and was given a posterior superior nerve block
(PSA), greater palatine nerve block and infiltration
around the teeth and appropriately anesthetized.
Intrasucular and vertical incisions were made with
a 15c blade and a full thickness flap was raised.
Osteotomy preparation began with the 2mm pilot
drill followed by the successive drills and since the
bone quality in the posterior maxilla was suspected
to be D3 the last drill was kept size lesser than the
desired implant width. After the osteotomy was
prepared long ADIN implant (Fig 2) was inserted
(Fig 3) achieving a primary stability of 35Ncm.
Cover screw was placed followed by sutures and
a baseline x-ray was obtained.
On the day of surgery the patient were prepared
and was given a posterior superior nerve block
(PSA), greater palatine nerve block and infiltration
around the teeth and appropriately anesthetized.
Intrasucular and vertical incisions were made with
a 15c blade and underlying alveolar bone was exposed by raising a full thickness flap. Osteotomy
preparation began with the 2mm pilot drill at
600rpm under saline cooling till a depth of 13mm
was done and an IOPA with the pilot drill was taken
which showed that the prepared depth was very
close to the sinus floor and the bone quality was too soft to widen the osteotomy further so we began
to condense the bone using osteotomes and so
the implant length was changed to 11.5mm along
with the sinus floor lift of 1mm was done using
the CONCAVE osteotome [JULL-DENT DENTAL
IMPLANT INSTRUMENTS & DENTAL IMPLANT,
MUMBAI]. Post the 2mm pilot drill the compacting
and bone expansion began using the 2.5 mm
osteotome (FIG 4 and FIG 5) till the depth of 11.5
using the stopper, followed by 3mm, and since
the quality was too soft the last width kept was
3.5mm 1 mm less than the desired implant width
where the osteotomes were inserted and rotated
simultaneously and were kept inside for 30 to
60 seconds to allow the bone to expand before
inserting the bigger diameter after going 1mm
deep with each osteotome xray was taken to check
the sinus floor and as we reached the sinus floor
osteotomes were tapped gently with the mallet
and if osteotome faced resistance further widening
was done. The valsalva maneuver was performed
was performed on multiple occasions to detect any
communication an no oroantral communication
was noted. Condensing and bone expansion was
achieved till depth of 11.5 and width 4.2, followed
by which the implant was inserted with a primary
stability of 35ncm, cover screws were placed and
flaps were sutured.
After the surgery all the subjects of each group
were asked to used ice pack to avoid any edema or swelling and were asked to refrain from blowing
vigorously through the nose, sucking through
straws to avoid increase or decrease in maxillary
air pressure. To prevent secondary infection of the
sinus and surgery site 500mg amoxicillin, Metrogyl
400mg Betadine rinse and 0.2% chlorhexidine
mouthwash was prescribed. Post 10 days the
patient was called for suture removal.
RVG was taken immediately(baseline) after the
implant placement, at 3 months and 3 months
post loading (Fig 6) to assess and measure the
bone level. X-rays were taken using long cone
paralleling technique (70kv, 10 mA, 0.2 seconds)
and x-ray was digitized using a specialized
software (SOPRO IMAGING SYSTEM version
2.0.272.0, size 4.27 MB) to avoid error each IOPA
was standardized using RVG SESNSOR HOLDER
[RINN XCP FILM HOLDER] (Fig 7, Fig 8) on which
patient putty bite was taken so that at each follow
up the sensor can be placed in the same position
and errors can be avoided.
The marginal bone loss will be determined by
measuring the distance from the implant abutment
interface to the first visible bone implant contact
(FBIC). Both mesial and distal sites were measured
separately and average values will be calculated.
(Fig 9) For more accuracy three readings were
taken and their average value were calculated. All
the calculations were performed by single clinician.
If the measured value is more than the previous
value there will be bone loss, if the measured value if less than the previous value there will be
a bone gain.
Software- SPSS version 20
Statistical tests: The Normality tests Kolmogorov-Smirnov and Shapiro-Wilks tests show that the data
is normally distributed. We conducted parametric
tests. Independent- t test was done to compare the
two groups, keeping value of significance p < 0.05.
Independent- t test: was used to compare the
difference between the mean of two independent
samples.
Comparison was done between groups A and B,
Groups C and D, Groups B and D.
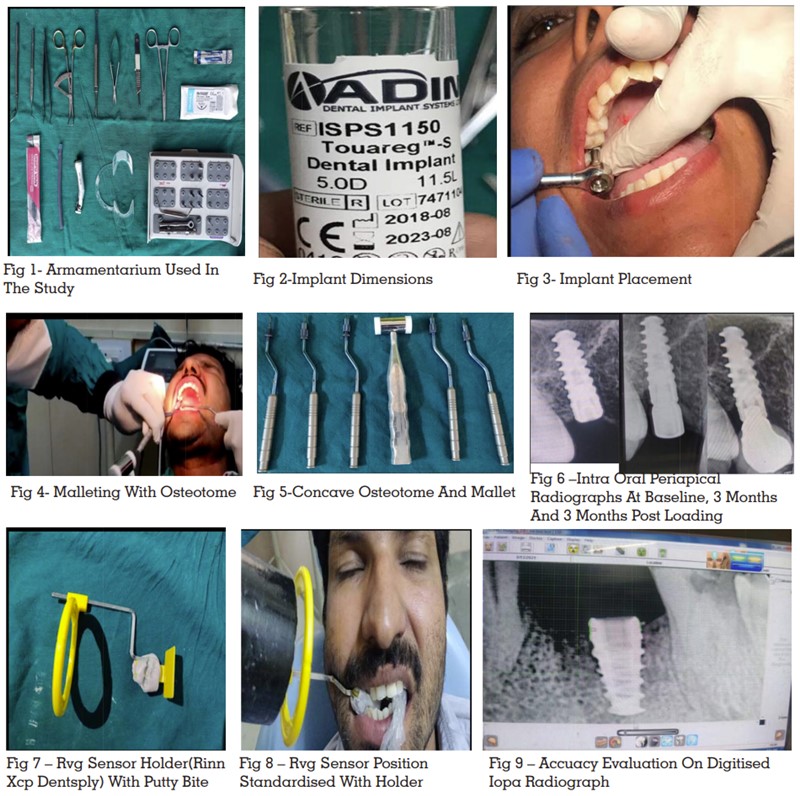
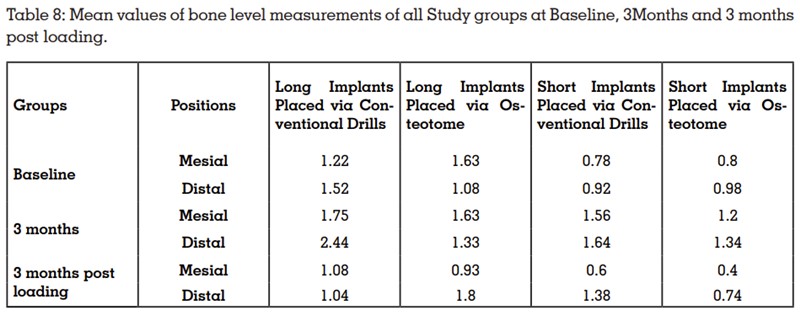
The readings for the groups A,B,C,D are
summarised below in the tables.
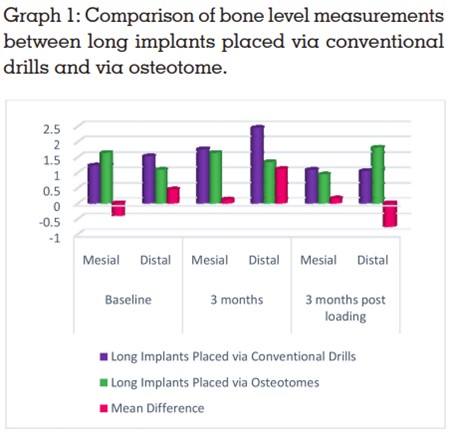
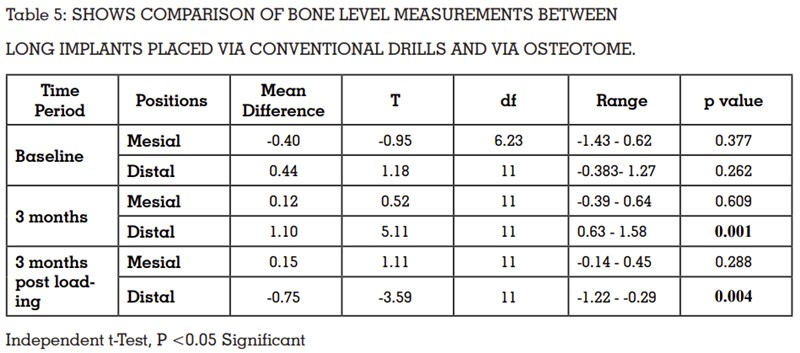
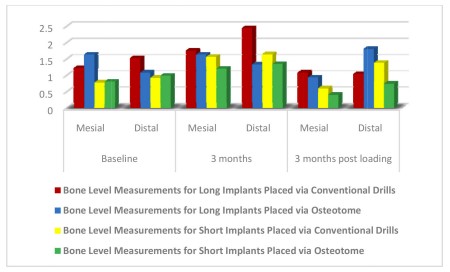
Inference: The results show that bone level
measurement at 3 months was higher at distal
position for long implants placed via conventional
drill compared to osteotome. The results were
statistically significant (p < 0.001).
At 3 months post loading, bone level measurement
was higher at mesial (0.15mm) position for long
implants placed via conventional drill compared
to osteotome. The results were not statistically
significant (p=0.288). The bone level measurement
at 3 months post loading was higher at distal
(0.75mm) position for long implants placed via
osteotome compared to conventional drill. The
results were statistically significant different (p
< 0.004).
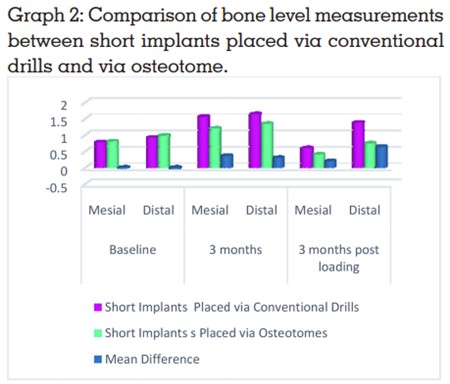
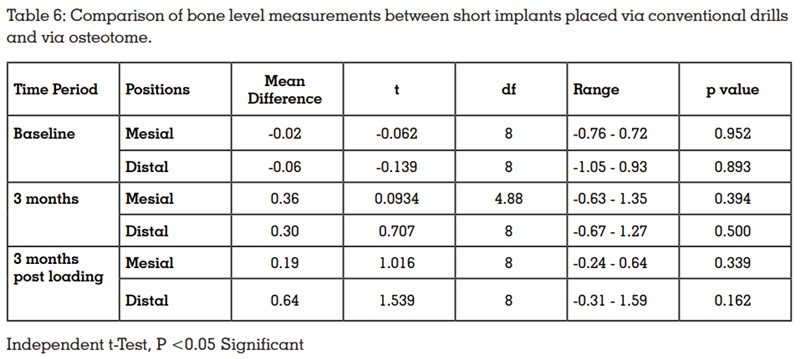
Inference: The results show that bone level
measurement at 3 months was higher at mesial
and distal positions for short implants placed via conventional drill compared to osteotome. But the
results were not statistically significant (p > 0.05).
At 3 months post loading, bone level measurement
were higher at mesial (0.19mm) and distal (0.64mm)
positions for short implants placed via conventional
drill compared to osteotome. But the results were not statistically significant different (p > 0.05).
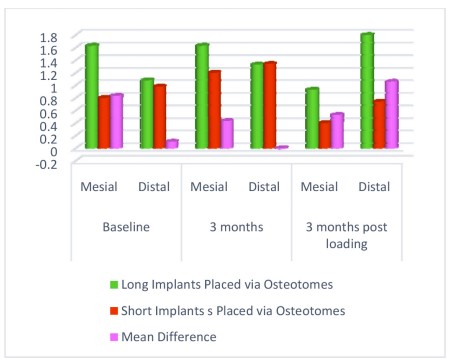
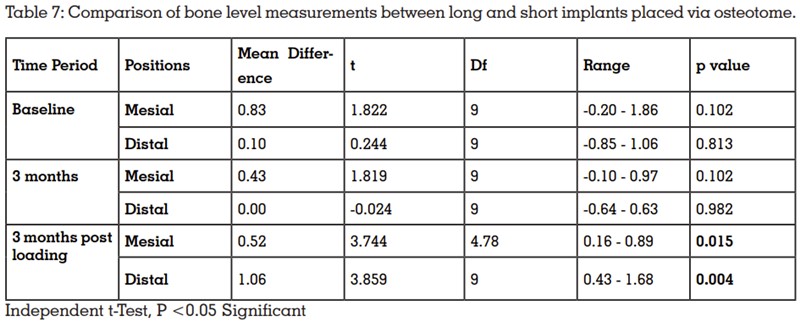
Inference: The results show that bone level
measurement at 3 months post loading were
higher at mesial (0.52mm) and distal (1.06mm)
positions for long implants compared to short
implants placed via osteotome. The results were
statistically significant (p < 0.05).
At baseline and 3 months, bone level measurement
was higher at mesial and distal positions for long
implants compared to short implants placed via
osteotome. But the results were not statistically
significant different (p > 0.05).
The posterior maxilla is one of the most challenging anatomic locations for the implant placement. The main reason for that is the pneumatization of sinus subsequent to the tooth loss. Vertical augmentation of the posterior maxilla has commonly been achieved by maxillary sinus augmentation. The main drawbacks of these augmentation procedures include morbidities such as post-operative infection, mucosal tissue breakdown, pain, bleeding, and neurosensory deficit. The alternative approach for the treatment of sites with vertical ridge deficiency has included short implants. Since the literature on short implants has some deficiencies, a thorough understanding about short implants becomes an important prerequisite before placing them.12,13,14,15,16 There are numerous classifications proposed for short implants17 but For the purpose of this case study 6th European Consensus Conference of European association of Dental Implantologists in 2011 approved the classification given by Olate which states implant as short if their length is <8mm, medium if between 9 to 13mm and long implant if > 13mm18.
ADVANTAGES OF SHORT IMPLANTS- Lower
cost, Less presurgical time and Costs for
surgery, can Avoid Complications that result
from advanced grafting procedures, Increases
patient’s acceptability, Less surgeries involved,
Fewer complications, Quicker rehabilitation time19.
Moreover when coming to the biomechanical
considerations for short and long implants both
it has been reported that long implants are
associated with more of biological complications,
where as short implants report more of technical
or prosthetic complications.20,21 Also less amount
of marginal bone loss has been reposted around
short implants due to “stress shielding” effect
occuring around short implants.
Surgical considerations for short implants –Two
stage surgery with delayed loading, eliminating
the countersink drill, soft drilling protocol.
Prosthetic considerations for short implants- internal
hex connection, platform switching, narrow occlusal
table, flattening cuspal inclines, eliminating
cantilevers, splinting implants22.
Short implants were associated with significantly
lower biological complication rates compared
with long implants placed after maxillary sinus
augmentation. Short implants were associated
with higher rates of prosthetic complications
compared with long implants23. Eight out of eleven
studies observed technical complications after 5
years in function, in particular screw loosening,
decementation.
The reason why we opted for osteotome technique
was because the poor bone quality and the
sinus pneumatization posed as obstruction for
rehabilitating the maxilla every time with a
standard length implant and drilling on top
of it lead to loosing the poor quality bone, so
osteotomes came to the rescue which are bone condensing instruments. Osteotomes are optimally
used by pressing the instrument into the bone and
malleting, ie, tapping the osteotome into place
with a surgical mallet only when there is slight
resistance. Firmer resistance may indicate the need
for wide-ning the cortex with a drill. Generally,
most resistance is caused by a cortical opening
that is too small for the osteo-tome to easily pass
through.25,24
Once the desired depth has been reached,
and before moving on to the next instrument,
it is advisable to wait 30-40 seconds for bone
microfractures to form and dilate and compact
the adjacent bone. So bone preservation, good
tactile sense to the operator, facilitating short
implant placement, avoiding complex grafting/
augmentation procedures as well as economic
are some of the advantages of osteotomes for
posterior atrophic maxilla. And as anticipated
osteotomes proved a very good technique to restore
the posterior maxilla with short implants in a quick
and precised way needless to say keeping the
occlusion and other biomechanical factors in
mind.26,27
When compared groups A (Long Implants placed
via drills) and B (long placed via osteotome) at
3 months post loading, bone level measurement
was higher at mesial (0.15mm) position for long
implants placed via conventional drill compared
to osteotome. The results were not statistically
significant (p=0.288). The bone level measurement
at 3 months post loading was higher at distal
(0.75mm) position for long implants placed via
osteotome compared to conventional drill. The
results were statistically significant different (p <
0.004). So, osteotome technique proves beneficial
for placing long implants.
When compared groups C (short implants placed
via drills) and D (short implants placed via
osteotomes). At 3 months post loading, bone level
measurement were higher at mesial (0.19mm) and distal (0.64mm) positions for short implants placed
via conventional drill compared to osteotome.
But the results were not statistically significant
different (p > 0.05).
When compared groups B (long implants via
osteotomes) and D (short implants via osteotomes)
The results show that bone level measurement
at 3 months post loading were higher at mesial
(0.52mm) and distal (1.06mm) positions for long
implants compared to short implants placed via
osteotome. The results were statistically significant
(p < 0.05).
Within the limitations of the study it can be
concluded that there was initial bone loss seen
at baseline and 3 months around both short
and long implants when placed via osteotome
technique which was statistically significant
however 3 months post loading the difference
was compensated around implants placed
via osteotome and the difference was not that
statistically significant. So the gain for long
implants via osteotome was statistically significant
making osteotome technique an advantage for
placing long implant but the low bone level for
short implants via osteotome was less statistically
significant making osteotomes and short implants
a beneficial and manageable protocol for highly
atrophied maxillary ridges.
LIMITATIONS OF THIS STUDY- The limitations
of the study are small sample size, less follow up
period so Suggestions for further research include
the demand for more longitudinal studies with
larger samples and longer follow-up times on
short and long implants. Osteotome technique not
to be used in type 1 and type 2 bone quality and
also in patients suffering with Benign Paroxysmal
Positional Vertigo [BPPV].