Aim: Esthetic rehabilitation of an orbital defect
with an orbital prosthesis using modified anatomic
mode of retention.
Background: Orbital deficits can result from
neoplasms, infections or trauma. These defects
lead to functional as well as esthetic disablement.
Prosthetic rehabilitation plays a vital role as an
alternative to surgical reconstruction in such cases,
as an orbital prosthesis provides a non-invasive,
cost friendly and esthetically predictable approach.
Retaining an orbital prosthesis within the defect
can be accomplished by various means such as
use of implants, adhesives or anatomic undercuts.
Engaging anatomic undercuts in the defect
ensures a practical, trouble-free, cost-effective,
and successful approach.
Case Description: In this clinical report we have
discussed a simplified approach to improve
the retention of an orbital prosthesis through
incorporation of an “acrylic plug” within the
prosthesis.
Conclusion: Conventional methods of retention of
an orbital prosthesis can be improved and modified
depending upon the anatomic and structural
attributes of the defect.
Clinical Significance: Conventional retention of
an orbital prosthesis can be enhanced in a cost
effective and time efficient manner as compared
to implant supported prosthesis.
Key words: Orbital defects, Orbital prosthesis, Retention in maxillofacial prosthesis.
Loss of a part of a body can have adverse
psychological and functional consequences.
Common indications for orbital exenteration
include neoplasms like basal cell carcinoma,
melanoma or squamous cell carcinoma; painful
blind eye; infection; recent injury; disfiguring blind
eye; prevention of sympathetic ophthalmia etc.1,2
The resultant defects can lead to esthetic as well
as functional impairment. For the reconstruction of orbit and the mid face, anterolateral thigh flaps,
fibular flaps and radial forearm flaps have been
utilized. An attempt at eyelid reconstruction is also
attempted many a times to increase the retention
of the prosthesis. Owing to the complexity and lack
of predictable outcomes, surgical management is
limited to coverage using microvascular free flaps.3,4
Hence, prosthetic rehabilitation plays a pivotal
role as an alternative to surgical reconstruction
in restoring the optimum esthetics and to improve
the psychological balance and social acceptance
of the patient. These prostheses also allow for
hygiene maintenance around the defect along
with observation for recurrence, if any. Retention
of these prosthesis is a major factor directly
related to the overall success of the prosthesis
as well as its acceptability by the patient. Various
modes of retention have been used to retain the
orbital prosthesis, such as implant supported
prosthesis, use of adhesives, spectacles, magnets
and anatomic undercuts. Anatomic undercuts
are mostly utilized for obtaining retention in an
orbital prosthesis owing to the technique sensitivity,
unpredictability, additional cost and comorbidities
associated with an implant supported prosthesis.5
An implant placement should be well planned
with an interdisciplinary approach, utilizing a
team effort of the maxillofacial prosthodontist and
the surgeon.6
Although implant-retained ocular prostheses play an important role in the success
of treatment, conventionally retained orbital
prostheses are practical, trouble-free, cost-effective,
and successful.7
Adhesives when used, can provide
satisfactory retention in cases where anatomic
undercuts are not present in the defect.8
Repeated
application and removal of the adhesive may result
in tearing of the margins compromising marginal
adaptability as well as the esthetics making the
prosthesis more conspicuous. In this case report
we have described a simple approach to improve
the retention of a silicone orbital prosthesis with
the use of an “acrylic plug”, in turn increasing the
acceptability and esthetic outcome.
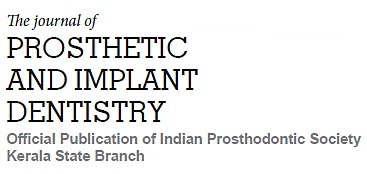
A 70-year old female reported to the Department of
Prosthodontics, with the complaint of unaesthetic
appearance due to deformity in relation to left
eye. The patient had a history of squamous cell
carcinoma followed by exenteration of the orbit
one year back. Careful examination revealed a
defect where the left eye once was, measuring
55mm medio-laterally, 48mm supero-inferiorly
and 15mm antero-posteriorly (Fig.1). Physical
examination of the defect revealed the presence
of an undercut in the inferolateral margin of the
defect. Hence, a silicone prosthesis engaging this anatomic undercut for retention was planned for
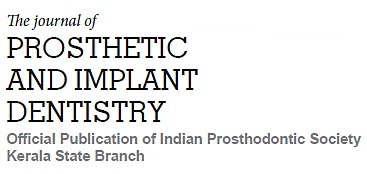
this patient. Firstly, an impression of the defect
was planned for the patient. An auto-polymerizing
acrylic (Rapid Repair, Pyrax Polymars, India)
customized tray (Fig.2a.) was fabricated for making
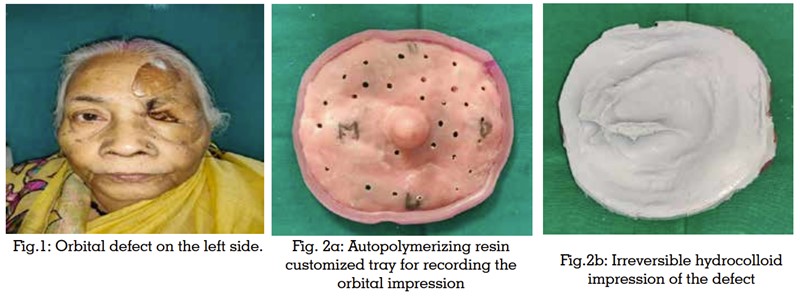
the impression with irreversible hydrocolloid
impression material (Tropicalgin, Zhermack,
Italy) (Fig.2b). This method improved the accuracy
and ease of impression making. The impression
was poured in type 3 dental stone (Kalabhai
Kalstone, Karson Pvt. Ltd., Mumbai) to obtain
the model. A PVC sheet (Easy-Vac Gasket, 3A
MEDES, Korea) of 1mm thickness was adapted to
the defect with the help of a vacuum former. This
served as a skeleton for the wax pattern improving
the adaptability as well as ease of try-in of the
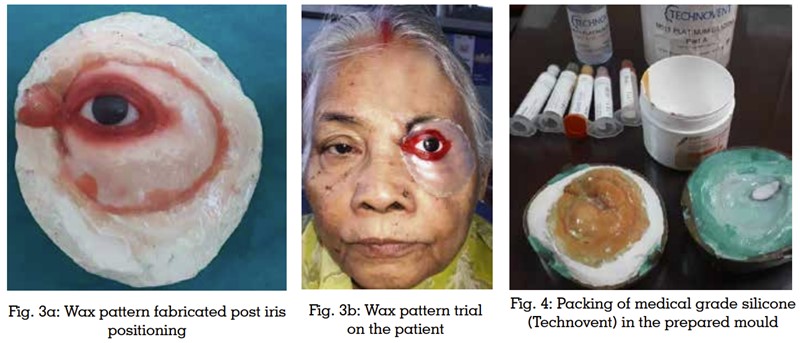
pattern. Following the adaptation of PVC sheet,
a stock scleral shell was used for iris positioning
within the defect. The iris positioning was done
in relation to the contralateral eye using the grid
method of positioning. After trial in the patient,
wax pattern was fabricated around this correctly
positioned iris (Fig.3a). The first structures to be
carved were the upper and lower eye lids. The
wax model was repeatedly tried on the patients
face and contoured keeping the adaptability, fit,
margins, and majorly, the esthetics in relation to the contralateral eye (Fig.3b). Once, the wax
pattern try in was satisfactory, a master mold was
made after investing the wax pattern. Following de-waxing, color matching for the silicone was done
using a spectrophotometer. The color matched
medical grade silicone (Technovent Ltd., UK) was
manipulated and packed in the master mold and
cured (Fig.4). The final prosthesis was retrieved
and finished with silicone trimming discs and
polished. The final prosthesis was tried on the
patient to evaluate the fit followed by extrinsic
staining to accentuate the esthetics of the final
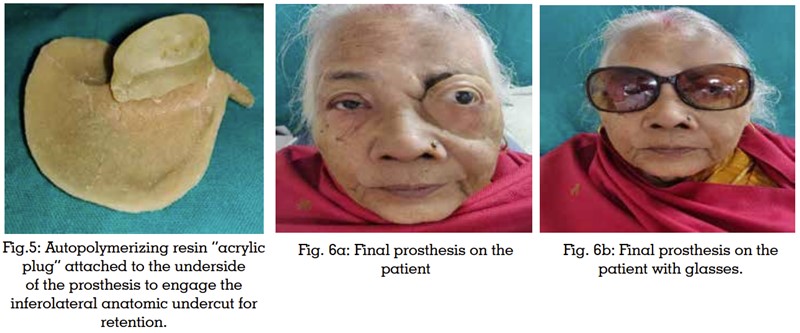
outcome. After the final trial, an acrylic plug was
fabricated by adapting the autopolymerizing
acrylic engaging the inferolateral anatomic
undercut (Fig.5). This plug was adapted throughout
the length of the undercut increasing the surface
area for enhanced retention. This plug was
attached to the undersurface of the scleral shell
through a tunnel created in the tissue surface of
the silicone prosthesis. This plug was then finished
and final try-in of the prosthesis was done in the
patient with and without glasses (Fig.6a & 6b).
Marked improvement in mechanical retention
was observed and the final esthetic outcome was
pleasing to the patient.
Amongst the facial prosthetic rehabilitation,
rehabilitating an orbital defect is considered
amongst the most difficult as the rehabilitation
aims at restoring a movable organ with a static
prosthesis. This is one of those esthetically complex
situations where obtaining adaptability, optimum
fit and retention along with esthetically pleasing
outcome becomes challenging. Various modes
of retention can be used for orbital prosthesis
such as adhesives, spectacles, magnets, and
maxillofacial implants. In terms of retention and
esthetic appeal, advanced treatment modalities
such as implant-supported orbital prosthesis
have a superior outcome but the cost is a major
constraint and hence not affordable for all
patients.7
Along with the financial limitations,
the second surgical exposure is another factor that
concerns the patients. Using anatomical undercuts
to obtain retention is one of the most economical
modes along with ease of fabrication.5
In this case
report, we have tried to increase the retention by
engaging the bony undercuts in the defect. Acrylic
plug improved the adaptability of the prosthesis
to the defect by improving the retention. This plug
can be modified and relined time and again based
on the retention requirements. Hence, there is an ease of fabrication and possibility for modification
according to the need and is an economic mode
of retention compared to the adhesives. Also, the
problems associated with cleaning the prosthesis
after use of adhesive leading to tearing and
inadaptability of margins is avoided.
Restoring orbital defects poses a challenge
for the maxillofacial prosthodontist in terms
of esthetic acceptance and retention of final
prosthesis. Amongst the various modes of
retention, utilizing anatomic bony undercuts of
the defect provides pleasing results with ease of
the fabrication procedure. In this technique, we
have laid out a simplified and economic approach
by incorporating an additional “acrylic plug”
attachment to enhance the retention and to provide
a possibility of modification depending on the
future needs. This prosthesis ensures adequate
retention affecting the psychological status of the
patient more positively.
Conventional retention of an orbital prosthesis,
using anatomic undercuts in the defect, can be enhanced in a cost effective and time efficient
manner as compared to implant supported
prosthesis. This saves patient the trouble of
undergoing another surgical exposure and the
additional cost and time associated with implant
placement.