Amputation is the complete removal of an injured or deformed body part. It usually occurs during a traumatic injury or due to surgical amputation. The rehabilitation of amputed finger depends on the amount of injury, amount of tissue and bone involved, location of residual finger and the esthetic and functional needs of the patient. Most of the finger prosthesis are designed for an esthetic purpose which help the patient to pass unnoticed. A good prosthesis should provide life like appearance to duplicate the missing structures which should meet esthetic and functional requirement of the patient. This article describes the steps in rehabilitation of an amputed finger and working principles and design of the flexible finger prototype.
Key words: amputation, finger prosthesis, functional finger prototype
Finger amputations can occur due to various
reasons such as accidents or explosions, severe
infections like untreatable vascular diseases or
malignant tumors. Amputations can occur directly
at the time of injury itself or as a result of surgical amputation when the surgical reconstruction of the
finger fails like in extensive damage cases where
finger cannot be restored. Amputations can cause
a great physcological and emotional trauma to the
patients, as it causes impairment of their skilled
and daily life activity. There are different types of
amputations which are self amputation, congenital
amputation, and traumatic amputation.1, 2, 3 The
prognosis of treatment for the rehabilitation of
the amputed finger or phalanx depends on the
following factors like amount of tissue and bone
involved, angles and levels of amputation and
involvement with other fingers. 4
An accurately fitting prosthesis should restore
normal length, protect the stump, maintain
sensitivity, transmits pressure and position
sense for doing various activities. Prior to the
treatment a proper evaluation of patient’s needs
and expectations, occupation, advantages and
limitations of final prosthesis has to be discussed
and taken into consideration. Different methods
of fabrication of esthetic finger prosthesis were
done in patients all these years. Most of them
had esthetics but lacked the functional ability of
the finger5-8.
The aim of the article is to introduce a new prototype
of functionally active economical flexible finger
prosthesis which could meet both esthetics and
functional requirement of the individual. This
article describes the steps in rehabilitation of an
amputed finger and working principles and design
of the flexible finger prototype.
Alginate Zhermack Tropicalgin, Hydrorise addition
silicone impression material putty consistency for
making impression, Hindustan modelling wax No:2
for making wax pattern, Stone gyprock dental stone
class III and Dental Plaster for making models.
DPI Heat cure Denture base material, DPI RR cold
cure acrylic for acrylisation, MP Sai enterprises
silicone for prosthesis and Acrylic paints for esthetic
designing, Wax knife, wax carver, rubber bowl,
camel haired brush for manipulation of materials.
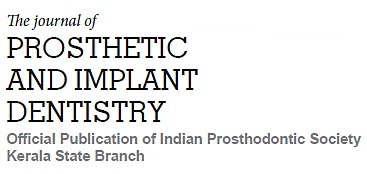
A patient of age 50yrs who was already
rehabilitated with esthetic finger prosthesis before
5yrs has reported back demanding for a flexible
functionally active finger prosthesis to meet his
occupational requirement. The steps in fabrication
of his previous prosthesis followed conventional
method which permitted minimal movements along
with his adjacent fingers connected by double ring. (Figure 1a, Figure 1b)
A new prototype was planned for making a
prosthetic finger with interphalangial movement
simulating flexion and extension like a normal
finger.
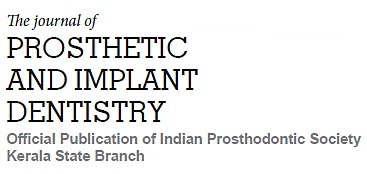
A proper case history and measurements were
taken which included the patient’s personal details,
dentist details, occupation of patient, reason for
amputation. A detailed case history mentioning
about the movement of amputed stump, width
of the bone end, pain and sensation of the area
were recorded. Affected fingers were correctly
marked, and measurement of corresponding finger
in the sound hand were taken, which included
measurement of distal, intermediate and proximal
phalanx. (Figure: 2a), total length of the nail of
corresponding finger on the sound hand was
measured (Figure: 2b), and following photographs
were taken for proper esthetic fabrication of the
prototype.
Palm and fingers on sound hand, Close up
photograph of fingers on sound hand, Dorsum
and fingers on sound hand, Close up of finger nails.
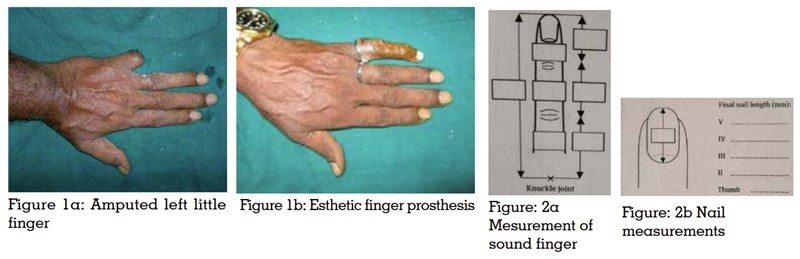
Alginate impressions of the amputed hand and
donor finger were made for making a mould.
Instructions were given to patient during impression
making like, hand should not touch the bottom
or walls of the tray during impression making, hand should be in functional position and finger
space is to be maintained. After obtaining the
cast proximal edge trim lines were marked on the
mould. Knuckle positions were marked on cast.
(Figure:2a, Figure:2b)
Fabrication of hollow wax pattern
Molten wax was poured into the impression of the
donor finger. A hollow wax pattern was fabricated
by placing a pencil in the centre of the mould by
applying petroleum jelly on it for easy retrieval
from the wax pattern. Pencil was held, above two
third the height of the distal phalanx in-order to
get the perfect morphology of distal phalanx.
The wax pattern of the donor finger was adjusted
and carved accordingly for the left little finger. A
wax trial of the prosthetic finger was done on the
stump of the amputed finger. The Measurements
of the wax pattern was reconfirmed again with the measurements of sound finger during trial, and
photograph was taken. (Figure. 4a)
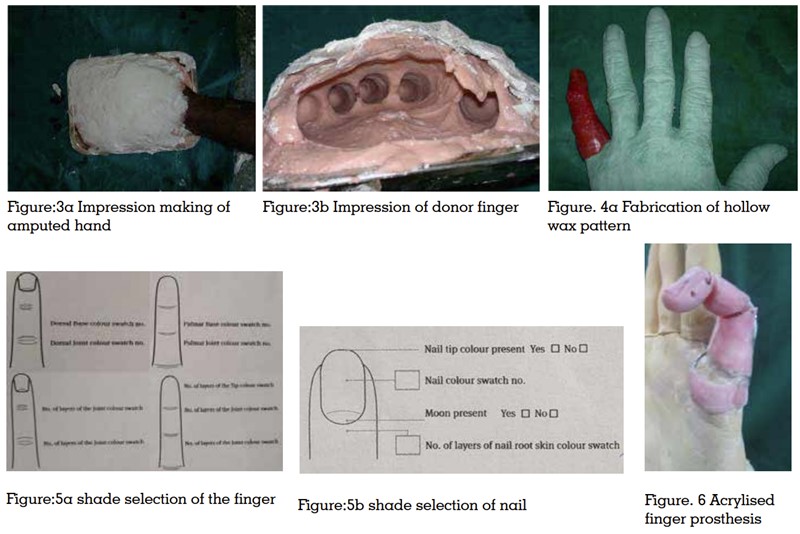
Shade selection of the following areas of the finger
was done during the trial. Dorsal base colour,
dorsal joint colour, palmar base colour, palmar
joint colour of the finger were taken. (Figure:5a).
Number of layer of joint colour of dorsal side and
number of layers of joint and tip colour on the
base skin of the finger were taken. Nail colour was
taken in following area. Tip of the nail colour, the
middle of the nail colour, whether moon present or
not, number of layer of nail root skin colour were
noted (Figure:5b).
After the necessary corrections were done on
the wax pattern, the interphalangial joints were
cut and made into three pieces, then two new
hinges in wax were attached in the interphalangial
joint regions. A wax pattern of retentive ring was made on the model, which was extended into
the proximal phalangial area and metacarpal
region. The entire prosthesis was acrylised. Each
of the phalangial halves were joined together with
orthodontic wires for flexibility and movements
were checked. (Figure. 6)
Trimming and polishing was done in necessary
areas for the smooth functioning of the prototype,
which was cut in the interphalangial joint area,
and was made into 3 pieces. Then acrylic hinges
were given in the innersurface of the hollow finger
at each interphalangial joint area. A retentive ring
was fabricated on the cast which encircles the
bottom portion of the amputed stump. Tightness
of retentive ring was adjusted with an orthodontic
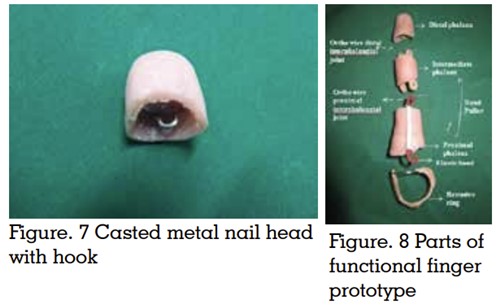
wire which was around the amputed stump. A nail
head was fabricated with cast metal alloy with a
hook positioned towards the interphalangial area.
The size of the casted nail head was reduced and
adjusted so that it correctly fits inside the acrylic
outer part of distal phalanx. (Figure. 7)
A sleeve for elastic band was attached to the
middle phalanx lengthwise. The elastic band was
inserted with the help of elastic band puller through
the sleeve. Then the finger was assembled to one
piece by connecting all the hinges in position
using 19-Guage orthodontic wire. The anterior
end of the elastic band was stretched and pulled
inside the hollow space of the middle phalange.
The other end was attached to the hook in the nail head inside the distal phalanx with the help
of customized band puller which was. Hence the
functional finger prototype was fabricated. (Figure.
8)
Principle of functional finger
The prototype is capable of flexing like a normal
finger by using the principle of gravity and elasticity.
When there is flexion or positional change of the
proximal phalanx, the casted metal-nail head
inside the distal phalanx will make the elastic
band which is embedded along the intermediate
phalanx of the prosthesis, stretch due to weight of
nail head and gravitational pull. This continuous
downward pull induces loss of elasticity of the
band and leads to the bending of the prosthesis.
On extension of the stump of the proximal phalanx
the elastic band gains its elasticity after a certain
positional change of the proximal phalanx. It
pulls back the casted metal nail head in the distal
phalanx making it straighten like a normal finger
Designing of outer covering of prosthesis
Designing can be done in two ways. 1) By gloving
the acrylic finger 2) By fabricating a silicone outer
covering for the prosthesis.
Gloving Method
In-order to reduce the cost factor, finger glove was
inserted over the acrylised prototype, and artificial
nail was made using self-cure acrylic resin and
fixed, glove was then painted using fabric paint
and was attached to the very minute hooks on
the retentive ring. This is a cost effective and less
technique sensitive method, but the colour stability
and durability of the prosthesis is less compared
to silicone outer covering. (Figure 9a)
Procedure for fabricating silicone prosthesis
Two impressions of the wax pattern of the finger
prosthesis were made and one was poured in
dental stone and other was poured again in wax.
The waxed model was used to create a mold space of the finger by lost wax technique. The stone model
was then reduced in size by trimming 2mm all
around for creating space for the passive vacuum
fit slicone cover. A putty is packed to lift the stone
model by 2mm in the anterior nail head region, for
the easy flow and packing of the silicone material
when placed inside the dental flask. (Figure. 9b).
The dorsal surface is in the lower part and palmar
surface is in the upper part of the flask. (Figure. 9c)
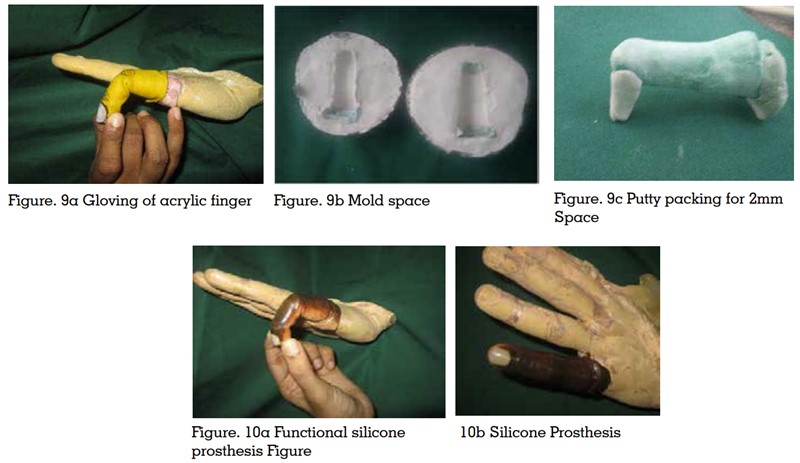
MP Sai enterprises room temperature vulcanizing
silicone is mixed and made to different shades
needed for making dorsal, palmar, knuckle joint
areas of the finger prosthesis and filled to space
inside the flask, which is then closed and allowed
to set for 24hrs. After complete curing it is then
trimmed and finished. Final color correction is done
by extrinsic painting in required areas. Artificial
nail is then made using self cure acrylic resin by
mixing with pink color acrylic to get appropriate
shade of the nail and which is then polished and
fixed to silicone prosthesis using cyanoacrylate
glue. (Figure. 10a), (Figure. 10b)
An ideal prosthesis should meet both esthetic
and functional requirement of the patient without
being too expensive, so that he can do his daily
activities. Several prosthesis available for finger
rehabilitation include esthetic acrylic finger which
is retained by structures like ring, Functional fingers
with interphalalgial movements, adhesive silicone
fingers, osseointegrated implant retained fingers,
Didricks X finger, Knicks prosthetic finger, Motorised
finger with biomedical neurosensors, M Fingers,
Pro Digit system, Vincent fingers etc. Custom made
acrylic finger prosthesis is a esthetic, cost effective
and less technique sensitive treatment. Patients
are initially satisfied but later find difficult as it
lack interpahalangial movements of normal finger.
Functional finger can be made by incorporating
small attachments inside the prosthesis in the joint
area.9-10 When the length of the residual finger is
very less only option which can provide retention
is the osseointegrated implants.
A study which compared esthetic and functional
outcome of adhesive and implant retained finger
found that esthetics, function and comfort is
more with implant retained prosthesis, but it is
not affordable for all patients because of higher
cost and surgical intervention required. Adhesive
retained is less expensive but has common
prosthetic complications like mild discolorations
and tear at the margin of the prosthesis11. The
term osseoperception described by Lundborget al
described the vibration and position sensations
acquired with osseointegration of implants.12
Rydevik et al proposed that implant retained
finger prosthesis allowed partial recovery of
tactile sensation by transfer of tactile stimulus to
inter-osseous nerves, because of direct pressure
of implant on bone.13 Popkong et al compared
one stage and two stage implant placement in
finger prosthesis and found that number of stage
depends on the primary stability of implant during
placement and condition of surrounding sift tissue.
Two stage has advantage of low risk of infection
and better soft tissue management, but one stage
has more patient acceptance because of earlier
prosthesis delivery and less surgical procedures.14
Marcello et al used used O-ring retention system
with modified hexagon shaped capsule adapted
to the acrylic resin to attach the prosthesis to the
implant.15
Didricks X- fingers are stainless steel the mechanical
fingers which are controlled by spring action. They
replace missing phalanges that are controlled by
the movement of the remaining portion of a finger
when available or by the movement of the hand
when no finger is available. They were usually used
to rehabilitate wounded US and British soldiers.
M fingers were introduced in 2009 by liberating
technologies for patients missing the entire finger.
Fingers are available as a kit, which was to be
assembled to address the index through small
fingers. Thumb is passive with a hinge that allows it to be manually prepositioned. Extension and
flexion of the wrist activate the device and pull the
cables attached to it and control the opening and
closing movement of the finger respectively. Each
finger has independent action when the individual
finger meets resistance it stops and others continue
which gives M finger a conforming grip around
an object. The strength generated by the user at
the wrist determine the force of the grip. Both X
finger and M finger are the body powered options
Knicks prosthetic finger are also foldable 3D
printed partial finger replacement device where
the movements are controlled by longer elastic
band attacing to the wrist area with an wrist band.
It is unaesthetic with less of patient satisfaction.16
Motorized fingers with biomedical neurosensors
are also available which can incorporate hand
motor function and feedback application. Array
sensors are incorporated to finger tips and palm
area to understand the amount and direction of
applied force, to know the point of application
of force on contact surface, to know the texture
of the object, to detect slipping for improving
grasping stability. Microfabricated tactile
sensors are developed to mimic one or all of the
properties human tactile system by simulating
machanoreceptors for pressure and vibration,
thermal receptors for temperature, nociceptors
for pain or damage.17-18
Prodigits (prosthetic digits) designed and
distributed by touch bionics are the first
commercially available powered finger with a
conforming grip. Fingers can be configured to
address any or all five missing digits. This device
is controlled by myoelectronic control and touch
pads. Myoelectronic control is by small amount
of electricity taken from remaining muscles in the
hand and forearm. Touch pad or force sensitive
receptors work on the pressure applied to a thin
pad by a portion of the remaining hand. It has
two input, one for opening and one for closing the fingers. This allows the user to have a conforming
grip around an object.
Vincent Finger system is designed by Dr Stephan
schulz, is currently undergoing clinical trials.
It is similar to Prodigits that each finger has
independent action and is powered by its own
motor is made from high strength, light weight
metal alloy. They are also developing Vincent hand
which is having a metal alloy chasis for mounting
five Vincent fingers and a sixth motor to control
thumb position. Both Prodigits and Vincent finger
system are externally powered options.19-21
This article describes the prototype of functional
finger prosthesis which is affordable for patients
of low economic status who have lost their middle
and proximal phalanx in accidents like crushing
away while using heavy machineries. The distal
phalanx has to be intact and in a movable
condition. Advantages include finger is functional
and esthetic with the matching skin color, the
cost of the finger can even be reduced if ordinary
glove is used instead of silicone. This finger can
be repaired and serviced by any dentist. Elastics
used are easily available and can be replaced by
himself or by a doctor. Prosthesis is light weight
and comfortable to the patient compared to
commercially available other functional prosthesis.