Cleft palate is a congenital facial deformity that presents clinically with anterior maxillary hypoplasia, congenitally missing teeth, nasopalatal communication, anterior open bite and a constricted maxillary arch. Aesthetic and functional rehabilitation of cleft palate patient requires the use of a prosthesis that provides adequate support to the lip and reduces the problem of nasal regurgitation. This article describes the fabrication of a removable prosthesis that has been modified anteriorly by providing added thickness to the labial flange so as to increase the lip support. This flange has been hollowed out to reduce the weight of the prosthesis and also provides comfort and ease of use. The palatal plate evades nasal regurgitation and improves speech.
Key words: cleft palate, hypoplasia, hollow prosthesis, rehabilitation
Cleft palate is a congenital fissure or elongated
opening in the soft and/or hard palate as a result
of improper union of the maxillary process and the
median nasal process during the second month
of intrauterine development. Any interference in
the normal embryonic development of face and
oral cavity can result in a cleft. It is a congenital
facial deformity with high incidence rate– 1 in 600
to 800 live births1
. Combined cleft of the lip and
palate has a higher incidence rate compared to
secluded clefts of lip and palate. It may occur
as an isolated entity or as part of a syndrome.
Approximately 70% of cleft lip and palate cases
are non syndromic2
and are considered to be of
multi factorial origin. This includes genetic predisposition and environmental factors such as
consumption of alcohol, smoking, intake of drugs
like phenytoin, maternal illness and many more,
which may influence embryonic development.
Depending upon the severity of interference to normal embryonic development, clefts may vary from the mildest ‘forme frustae’ of the lip or submucous
cleft of the palate to complete cleft extending from
lip, through ridges hard palate and soft palate3
.
One of the oldest system of classification was put
forward by Davies and Ritchie in 1922 and Veau
in 1931. Veau in his publication ‘Division Palatine’ describes four forms of cleft palate based on
morphology. Since then numerous classification
systems were described including symbolic representations (Schuchardt and Pfeifer, 1964), use
of acronyms (LAHSN, LAPAL 2007), diagrammatic
representations (Lima clock diagram, 2009), etc to
organize data and simplify treatment planning.
A universal structured form for description of cleft
lip and palate phenotypes is the CLAP notation
which is an acronymic shorthand for the longhand
structured form. Uppercase letters summarize
the part of the anatomy involved and lowercase
prefixes and suffixes are added to describe the
pre foraminal and post foraminal morphology.
Cleft lip with or without cleft palate occurs due
to incomplete fusion of medial nasal, lateral nasal and maxillary processes on both sides. The
site of the cleft theoretically corresponds to the
lines along which the embryonic processes fuse
together. Usually the cleft develops between the
lateral incisor in the premaxilla and canine in
the lesser segment. There is almost always a
‘pre-canine’ tooth on the lesser segment. If the
premaxilla contains a lateral incisor it is generally abnormal and is situated above the level of
the central Incisor. It tends to be undersized and
decayed looking often protruding out sideways. At
times it emerges high inside the cleft at the level of
the nostril, which is usually removed in the course
of lip surgery. Another feature is the presence of
supernumerary lateral incisors labial to the cleft
site in both deciduous and permanent dentition.
Neonatal teeth are also seen which may exfoliate
from the greater segment.
The cleft widens after birth and this is due to distorted traction of the facial muscles and the pressure exerted by the tongue. The width of the cleft increases anteroposteriorly from the free border
of the lip to the anterior palatine foramen and
posteroanteriorly from the uvula to the anterior
palatine foramen. This can be controlled by appropriate surgical procedure at the right age due
to the altered growth pattern. However, abnormal
facial growth pattern such as gross maxillary
arch contraction, midface retrusion and poor facial growth are usually noticed in patients with
repaired cleft lip and palate. To reduce the deleterious effect of surgery on facial growth, Gillis
and Fry, advocated delayed hard palate closure.
According to this regimen the closure of the soft
palate is carried out and a prosthetic obturator is
placed, which delayed closure of hard palate4
.
Further studies have concluded that palatal surgery in infancy has the potential to cause severe
midface retrusion and mandible is both smaller
and retropositioned5, 6.
The hypoplastic maxilla often results in a sunken
appearance of the midface which may be corrected
by both invasive and noninvasive procedures.
Treatment options may range from Le Fort 1 surgery
and distraction osteogenesis to the use of removable prosthesis. Combined fixed and removable
prosthesis can also be successfully employed for
anterior maxillary defect7. When only few natural
teeth remain removable prostheses retained with
telescopic attachments8
or overdentures9
provide
satisfactory results in retention of the prosthesis.
But the restoration of bone and soft tissue defect
in the anterior region of the face poses aesthetic
challenge in successful rehabilitation.
Here an added thickness of acrylic employed in
the labial flange region of a removable prosthesis
provides an easy solution for anterior maxillary
insufficiency without the need for any complex
attachments. But often the added thickness and
weight anteriorly can result in easy dislodgement
of the prosthesis during physiologic movement.
This case report presents the prosthetic rehabilitation of a repaired cleft palate patient with severe
maxillary hypoplasia rehabilitated with a removable prosthesis that is hollowed out anteriorly to reduce the weight of the prosthesis.
A 70 year old female patient reported to the Department of Prosthodontics, Government Dental
College, Thiruvananthapuram with the chief complaint of difficulty in speech, nasal regurgitation
of food and aesthtics (Fig 1). On examination, it
was found that the patient had a residual cleft of
the anterior alveolus involving primary palate,
belonging to category 1b of American Cleft Palate-Craniofacial Association (ACPA) classification10.
There was no evident residual cleft in the hard
palate as she had undergone a series of surgical
repairs prior. Intraoral examination also revealed that the maxillary arch was severely constricted
such that the entire maxilla was contained within
the mandible (Fig 2). She had only few posterior
teeth remaining which were palatally placed in
relation to mandible and were not able to establish
occlusion with the opposing arch. The mandibular
arch had full compliment of teeth upto second
molar on both sides, except the root stump of the
left first molar. The palatally placed teeth had
short mutilated crowns which were periodontally
compromised and cannot be utilised for retention
purposes. Hence it was decided to relieve the
respective teeth in the denture base.
The patient’s primary concern was about the unsupported nature of the upper lip and the sunken anterior region beneath the nose. She had been
wearing a removable prosthesis ever since her
younger days and hence willing to accept a removable prosthesis that would make her speech legible and also provide adequate fullness to the lip.
Preliminary impression was made using irreversible hydrocolloid in a stock tray and primary casts
were poured. After blocking out the teeth and
undercuts present, a custom tray was fabricated
using self cure acrylic resin. Border moulding and
final impression was carried out subsequently and
a master cast was poured with dental stone. During
the jaw relation appointment special attention was
given to provide added thickness of wax labially
as per the patient’s demand (Fig 3). The patient had an anterior open bite and posteriorly, few
natural teeth contacted the opposing arch. The
excessive thickness of wax anteriorly was found
to be a challenge in retaining the prosthesis in the
patient’s mouth. The existing natural teeth had
short clinical crowns which did not facilitate clasp
placement. Hence it was planned in such a way
that the labial flange be made hollow to reduce
the weight of the prosthesis and also to extend
into the buccal sulcus for extra retention and at
the same time providing adequate fullness. After
evaluation of jaw relation and try in the denture
was finished and polished (Fig 4 and 5).
The waxed up denture was invested and dewaxed
in a conventional manner (Fig 6). Then steps were
taken to produce a hollow labial flange.
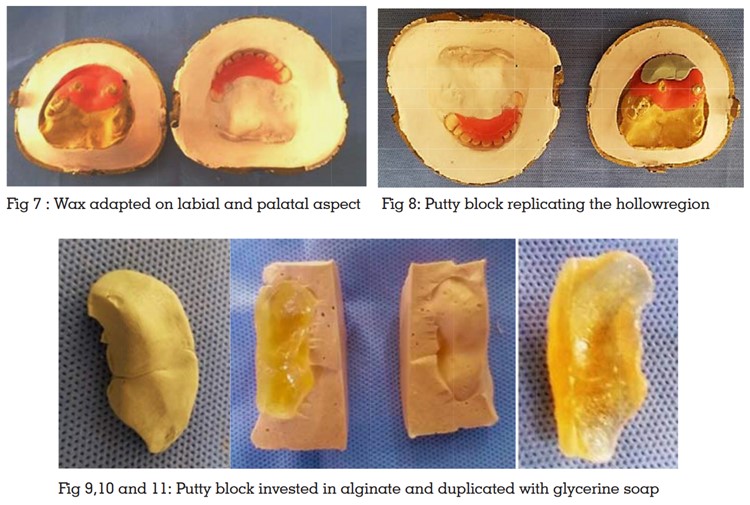
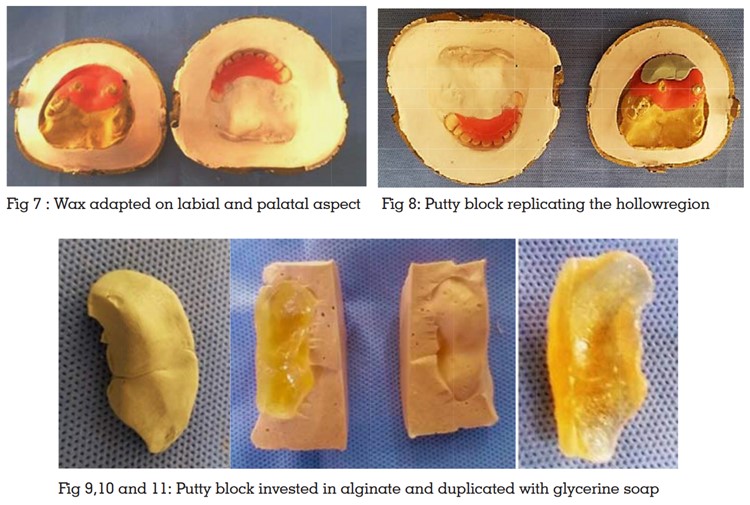
To provide uniform thickness of acrylic resin around the hollow space two strips of wax where adapted
on the labial and palatal aspect of the mould
corresponding to the labial flange (Fig 7). A putty
block was placed in the mould corresponding to
the labial flange region and the flask was closed
to replicate the shape of the hollow region (Fig 8).
The set putty block so obtained was invested in
alginate and duplicated in glycerine soap (Fig
9, 10, 11).
After packing a small amount of acrylic resin on
the labial and palatal side of the labial flange the
initial putty block was placed and the trial closure
was done. Once the flask was opened, it was ensured that sufficient thickness of resin was present
along the margins of the hollow space (Fig 12).
Then the putty block was replaced with soap and the flask closed and cured in conventional manner. After curing the denture was trimmed and
finished. Two holes were made on the palatal
surface of the labial flange and the denture was
kept immersed in water to dissolve the soap. Final
cleaning of the hollow cavity was done by injecting
water through one hole and the remnants of the
soap exited through the other hole. After thorough
removal of soap, the holes were closed using self
cure acrylic resin. This lightweight prosthesis was
then delivered to the patient (Fig 13). Moreover the
cusil nature of the denture enhanced the retention
and comfort considerably (Fig 14 and 15). The
patient was satisfied with the aesthetics as well
as with the better articulation of speech achieved
with the new prosthesis (Fig 16 and 17).
Multi-disciplinary team approach in the management of cleft lip and palate is well recognised.
The role of a prosthodontist in dental care is to
restore appearance and function where surgery
and orthodontics had failed to provide optimum
results. This encompasses restoration of the health
of remaining teeth, replacement of missing teeth,
maintenance of arch form, obturation of naso palatal communication and improvement in speech.
One of the most challenging aspect of cleft lip
and palate rehabilitation is the restoration of normal facial appearance in maxillary hypoplasia.
The impaired growth in the maxillary anterior
region, especially after multiple surgical protocols
can result in anterior maxillary insufficiency. The
tooth and bony defects in the cleft side include
hypoplastic teeth, hypodontia, deficiency of alveolar bone and palatal or buccal fistulae. This
often compromises the surgical and orthodontic
treatment necessitating prosthetic intervention for
achieving reasonable results. The scarring following surgery results in a practically inactive upper
lip which fails to conceal any alveolar defects or
irregularities in gingival contour. Same time it acts
as a hindrance to the extension of labial flange
into the sulcus. The lip is generally unsupported
due to the underlying extensive dental and skeletal anomaly and often requires support with a
prosthesis.
Fixed, removable and implant prosthesis may be
employed as prosthodontic treatment options in
cleft palate rehabilitation. Extensive fixed restorations were advocated earlier under the belief that
it would stabilize the entire arch11. But currently
conventional crown and bridge work is advocated
when the edentulous span is small and the bridge
work does not run across the cleft. Less extensive
fixed restoration with one or two abutments on
either side of the cleft12 also may be attempted.
Adhesive restorative techniques such as resin
composites, porcelain laminate veneers, Andrews bridge and resin bonded fixed partial denture13,
may be used in younger adults for whom minimal
tooth preparation is essential.
Dental implants may prove to be useful in edentulous patients to enhance retention. They also
serve to replace missing congenital teeth but the
major problem with this treatment modality is the
difficulty in finding adequate bone of good quality.
Zanolla et al evaluated the longevity of prosthetic
rehabilitation treatment with implant-supported
overdenture (IOD) and implant- supported fixed
denture (IFD) in cleft lip and palate patients over
a period of 22 years and concluded that the success rate was not compromised and resulted in
satisfactory longevity. But the maintenance of the
prosthesis was challenging due to wear of the teeth
and recurrent fractures14. A retrospective study on
implant borne prosthetic rehabilitation in cleft lip
and palate patients have found that implants are
a reliable prosthetic option for such patients15.
A removable prosthesis such as a tooth supported
overdenture can be successfully employed to enhance retention and improve speech and function16.
But this treatment option requires the abutment
teeth to be in excellent periodontal health and free
of caries. Periodic follow up and meticulous oral
hygiene practices are mandatory to maintain the
periodontal health of the abutments.
The cleft palate patient discussed here presented
with short clinical crowns, unfavourable location
of teeth and a flat palate. Arch discrepancy in the
form of Angle’s class III occlusion, reverse overjet
and buccal crossbite accompanied by an anterior
open bite were also present. Moreover the presence of very few existing teeth with periodontally
compromised condition precluded successful rehabilitation with a fixed dental prosthesis or an
overdenture. The non availability of adequate
quantity and quality of bone at the anterior region
excluded rehabilitation with implants. Hence a
removable prosthesis option was selected which
served to obturate palatal defects, disguise arch discrepancies and replace missing teeth.
The treatment plan should be customised based
on each patient’s necessities and aesthetic requirement concomitant with a multidisciplinary
approach. Hollowing of obturator or complete
denture prosthesis using various materials and
techniques has been abundantly described in
literature. Some of the commonly used materials
include sugar17, salt, gelatin18, thermocol, polyurethane foam19, wax or acrylic shim, silicone20, 21
etc. A hollowing technique using gelatin soap
has been adapted here considering its ease of
retrievability and ability to withstand the curing
temperature of acrylic resin22. The added thickness
of labial flange given in the current prosthesis
serves to satisfy the esthetic requirement of the
patient. The hollowing of the labial flange resulted
in a lightweight prosthesis enhancing the comfort
and ease of use. The unfavourable location of
the few existing natural teeth in the maxillary
arch prompted the need for a complete denture
base with appropriate relief in the regions corresponding to the respective teeth. The prosthesis
discussed here satisfies all the functional and
esthetic requirements of the patient and provided
acceptable prosthetic rehabilitation.
Effective teamwork between the prosthodontist,
dental technician, speech and language therapist
and patient’s family is essential to assess the
prognosis for each patient. Successful rehabilitation of a cleft lip and palate patient depends
upon the extent of the defect, anatomic limitations
and patient motivation. A dental prosthesis that
is acceptable to the patient should be convenient
to wear, maintain arch form, provide adequate
function and evade social stigma.