The art of reconstruction of the defects by non-living substitutes is the heart of maxillofacial prosthodontia1
. Reconstruction of any facial defect is a
challenging task as a clinician. The prevalence of
the eye defects has been reported to be about 60%,
majority of which have been amongst the males.2
The loss of an eye may be due to a congenital
defect,tumour,trauma. Rehabilitation of such complex defects requires a customised approach for
the successful outcome of the prosthesis2.
Peymen et al. has classified the surgical management of the removal of eye as: evisceration,
enucleation and exenteration. Rehabilitation of
the orbit with lost volume can be done either by a
surgery or with the help of a prosthetic device3
. A
craniofacial prosthesis that replaces the eyeball
is an orbital prosthesis whereas the one which
replaces the surrounding periorbital tissues is an
ocular prosthesis. An accurate management for
a successful rehabilitation involves a multidisciplinary approach4
This case report presents a practically convenient
procedure for the construction of a customised
orbital prosthesis that is aesthetically pleasant,
retentive, and cost-effective. Here, the management
following an enbloc removal of an eye was done
using an adhesive retained silicone prosthesis.
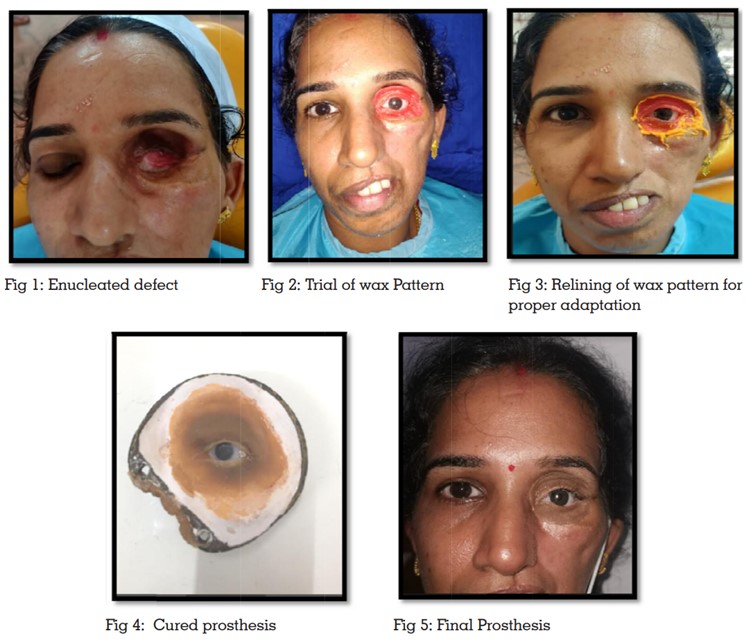
A female patient aged 38 years, reported to the
Department of Prosthodontics, complaining of
a missing left eye with a history of low-grade
adenocarcinoma of left maxilla. After correction
of post maxillectomy defect, she presented with
ectropion of left eyelid and plate exposure along
the infraorbital margin which was reconstructed.
She then underwent left eye enucleation (fig:1).
Enucleation is the removal of the entire globe
by cleaving all blood vessels, nerves along with
muscles adhered to the orbit3.
On Clinical examination, a left side orbital defect
was seen. The defect did not have any definite
hard and soft tissue undercuts to aid in retentionor the prosthesis. The treatment involved rehabilitation using medical grade silicone retained with
an adhesive.
The operator can choose from myriad options available for rehabilitation. However, the prime factors for an organized treatment plan include patient’s health, financial stability, involved tissue conditions and the technical skill. The fabrication involves the following sequence:
After the initial examination and inspection of the
defect, the socket was cleaned by irrigating with
saline. The eyebrow and eyelashes were lightly
lubricated prior to impression making. Primary
impression of the defect area was made using an
irreversible hydrocolloid (Tropicalgin, Zhermack).
Modelling wax was placed around the defect
for boxing (The Hindustan Dental products, Hyderabad, India). Alginate was then painted lightly
and carefully into the area of the defect. Then the
boxed area was entirely filled with alginate. The
positive replica of the defect was made using type
III Gypsum (Gem Stone, Shruti Products, Gujarat,
India).
Various modes of retention for maxillofacial
prostheses include magnets, spectacles, tissue
undercuts,adhesives and osseointegrated implants5
. Since the bone density was less and the
bone quality was inadequate, an adhesive retained prosthesis was the preferred option. The
silicone used in the prosthesis had a life like appearance and had precise margins which could
easily merge into the patient’s skin6.
Orientation of the stock shell was done while involving the right eye in a conversational gaze (fig.
2). The contralateral eye was used as a guide to
select and match the prefabricated eye shell. The
required landmarks were ascertained by positioning the iris and the patient such that he had a
straight line of vision. After the initial orientation,
layers of wax strips were appended to imitate the
contralateral eye giving it life like appearance. The
interlid space, wrinkles and the upper and lower
eyelids were precisely sculpted and contoured.
The pattern in wax was then assessed on patient
appraising the position of the eye shell, aperture
width of lids, and final adaptation. The wax pattern was then relined for precise margins and
adaptation (fig :3).
Following the wax try-in, it was reverted to the
working cast which was then invested. To prevent
the displacement of the eye shell, it was carefully
secured with acrylic indexing. Flasking and dewaxing was done meticulously for the retrieval of
the eye shell without any damage. Uncoloured
RTV medical grade Silicone (A-2186, factor II INC.
Lakeside, USA) and liquid catalyst was weighed
on a weighing machine. The required amount
was then mixed thoroughly to prevent entrapment
of air. Some intrinsic stains (Functional Intrinsic
Skin Colors, Factor II, AZ,USA) were added at the
time of packing for enhanced shade matching.
Silicone was then packed in layers and cured for
48 hrs. After deflasking, the final prosthesis was
retrieved followed by the incorporation of some
extrinsic stains (fig:4). The vignette of this prosthesis was achieved by positioning the artificial
superior eyelashes giving it an authentic and
graphic appearance.
The prosthesis was placed, and the patient was
instructed on the procedure of insertion for the
prosthesis by footing the orbital prosthesis in its
position (fig:5). This prosthesis came about to be
satisfactorily retentive as well as up to her wonted
appeasement. The spectacle frame was used
as an aid for additional retention and stability.
Instructions regarding the maintenance and the
follow up care was clearly explained to the patient.
Unacceptable facial disfigurement following an
orbital defect could be traumatising to a patient.
Its thereby essential to boost the patient’s morale
by combating the psychosocial trauma. A multidisciplinary approach should be followed to
successfully rehabilitate such patients using the
appropriate material, retentive aids, and based
on the functional and aesthetic requirements of
the patient. Here, an adhesive retained orbital
prosthesis was delivered to the patient to restore
the confidence to face the world.