Amelogenesis imperfecta is a congenital disorder which affects deposition, calcification and/ or maturation of dental enamel. This genetic disorder affects teeth in both deciduous and succedaneous dentition leading to functional as well as esthetic inadequacies. This condition exerts radical repercussions on stomatognathic system and intangible effects on the confidence of the patient. This clinical report elaborates on the multidisciplinary approach adopted for full mouth rehabilitation of a dentition affected by this genetic disorder in young adult patient. The treatment plan aimed at upheaving esthetics, restoring the vertical dimension and reinstating the masticatory function. Pankey–Mann–Schuyler philosophy of full mouth rehabilitation was adhered to achieve these treatment objectives. Full mouth rehabilitation albeit restoring esthetics and function also imparts a substantial positive psychological upliftment and therefore revamps the patient confidence.
Key words: Amelogenesis Imperfecta, Full Mouth rehabilitation, Pankey-Mann-Schyuler philosophy, Broadricks Occlusal Plane Analyser
Amelogenesis imperfecta has been described
as a complex group of genetic disorder that
primarily affects the enamel structure and exists independent of any related systemic disorder.1–2
Both deciduous and permanent dentitions are
affected by this enamel anomaly.3
It is entirely
ectodermal, and the mesodermal components of
the teeth are unaffected. Amelogenesis imperfecta
trait can be transmitted either by autosomal
dominant, autosomal recessive or X-linked
mode of inheritance. It is caused by mutation or
altered expression of genes such as: enamelin,
ameloblastin, tuftelin, MMP-20, and kallikrein.2
Amelogenesis imperfecta [AI] can be broadly
classified into four primary groups based on
phenotype—hypoplastic, hypomaturation,
hypocalcified and hypomaturation-hypoplastic.
However, at least fifteen subsets of amelogenesis
imperfecta have been identified when phenotype
and mode of inheritance are considered3
. Clinical
findings of AI include, enamel deficiencies, root
malformations, impaired tooth eruption, pulpal
calcifications, impaction of permanent teeth,
progressive root and crown resorption, congenitally
missing teeth and tooth sensitivity. Since enamel
thickness is severely affected, teeth are undersized
with prominent spaces between the adjacent teeth,
compromised oral hygiene and mouth breathing
with associated gingivitis, gingival hyperplasia and
other periodontal problems. Other clinical findings
associated with amelogenesis imperfecta include
congenitally anodontia, open occlusal relationship,
multiple impacted teeth and taurodontism.4
Management of amelogenesis imperfecta is
quite challenging and arduous to accomplish.
Comprehensive treatment planning shouldn’t
be undermined and the critical procedure in the
treatment planning is the evaluation of vertical
dimension using mounted diagnostic casts and a
diagnostic wax-up. Age of the patient, type and
severity of the disorder, socioeconomic status
and intraoral condition at the time of treatment
planning are some of the influential factors that
impact the treatment planning in such patients.
The final objective of the treatment plan should
be to weave esthetics, masticatory function and
general oral health into harmony.
The rehabilitation of entire dentition for patients
with amelogenesis imperfecta can be achieved
successfully by using the philosophies of full
mouth rehabilitation. They provide tangible and
everlasting esthetic result in tandem with occlusal
harmony. Full mouth rehabilitation procedures
are a complex set of procedures which restore the
teeth to their natural form, function, and enhances
esthetics in harmony with the temporomandibular
joint and the associated hard and soft tissues.5-6
Although several philosophies and protocols
have been widely documented, two of them are
routinely employed. They are, Hobo’s twin stage
technique and Pankey-Mann-Schuyler (PMS)
technique. This clinical case report illustrates the
treatment procedures carried out sequentially in a
full mouth rehabilitation using porcelain fused to
metal crowns strictly adhering to Pankey–Mann–
Schuyler philosophy in a patient with dilapidated
dentition due to amelogenesis imperfecta.
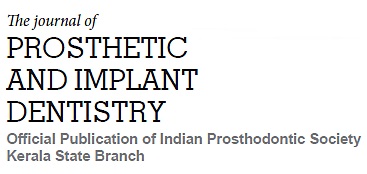
A 22-year-old female patient reported to the
Department of Prosthodontics with a chief
complaint of generalized discolouration & stained
appearance of her teeth. She also expressed
concerns regarding her teeth size, shape and
shade along with poor masticatory efficiency [Fig 1]. The patient had no history of any major systemic
illnesses. Clinical and radiographic examination
of the patient revealed no abnormality in
temporomandibular joint movements, generalized
mild attrition and discoloured teeth with irregular
pattern of mineralisation. The patient did not
have any loss of vertical dimension of occlusion.
Based on the clinical and radiographic findings,
the patient was diagnosed with amelogenesis
imperfecta and the patient was advocated for
full mouth rehabilitation to address her chief
complaint.
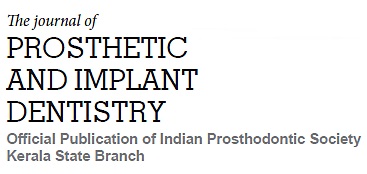
Preliminary impression of maxillary and
mandibular arch was made using irreversible
hydrocolloid and diagnostic casts were mounted
on a semi-adjustable articulator using interocclusal
record after a facebow transfer. Protrusive record
was obtained from the patient to program the
articulator.. Preliminary analysis was carried
out on the mounted casts followed by diagnostic
wax-up without altering the vertical dimension
was performed on the maxillary and mandibular
anterior teeth [Fig 2].
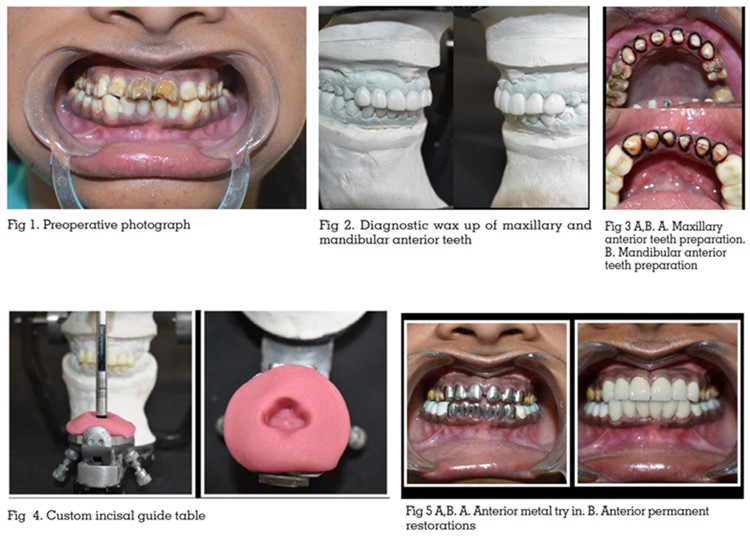
After preparing the maxillary and mandibular
anterior teeth [Fig 3] the provisional crowns
which were fabricated using the putty index of the
diagnostic wax-up were luted using a provisional
cement. The provisional restorations given to the
patient were utilised to assess the anterior esthetics
and help determine the anterior guidance for the
patient. Once the patient got accustomed to the
established anterior guidance, a custom incisal
guide table was fabricated on the articulator [Fig
4]. The final restorations for the maxillary and
mandibular anterior teeth were fabricated and
cemented after metal try-in procedure [Fig 5].
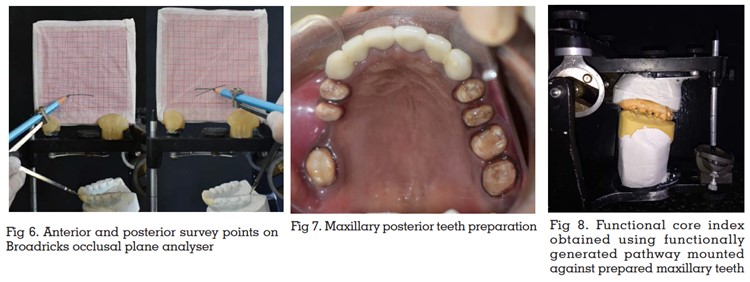
The subsequent procedure was to restore the
mandibular posterior teeth. Diagnostic wax-up of
mandibular posterior teeth was performed on the
mounted cast prior to preparation of teeth in the
patient. The occlusal plane and Curve of Spee were
established by using Broadricks Occlusal Plane
Analyser [Fig 6]. Then, to fabricate the provisional restorations, putty index of the wax-up was made.
The temporary crowns fabricated were cemented
provisionally after teeth preparation. Tooth
preparation and provisionalization of mandibular
posterior teeth were completed segmentally.7
Patient’s occlusion and comfort were evaluated for
the next three weeks. When provisional restorations
were considered acceptable, they were used to
develop form and contour of definitive restorations
for the mandibular posterior teeth. The final
restorations of the mandibular posterior teeth
were cemented and succeeded by the fabrication
of maxillary posterior restorations using the
functionally generated pathway [FGP] technique.
The maxillary posterior teeth were prepared [Fig
7] and a final impression was made to obtain the maxillary master cast. Centric relation record was
made and utilised to mount the maxillary and
mandibular casts to the articulator. The patient
was asked to perform the centric and eccentric
movements which were recorded using functional
wax. This provided the FGP record. Quick setting
plaster was poured into this record to obtain the
functional core index which was articulated against
the maxillary master cast [Fig 8] to develop the
wax patterns for maxillary crowns in group function
occlusion. After a bisque trial, final restorations
were luted and group function occlusion was
achieved. [Fig 9]
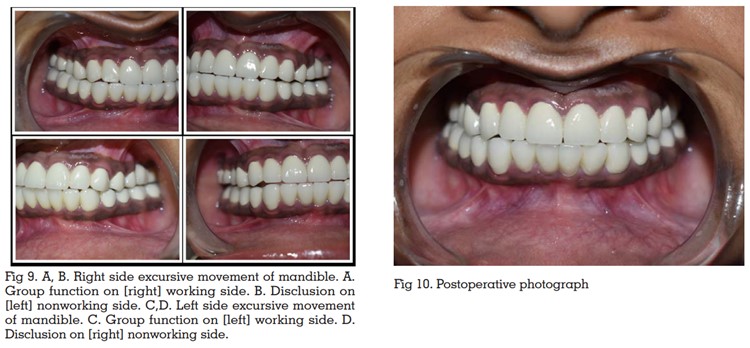
Regular recall and review protocol were effectively
employed and oral hygiene maintenance instructions were reiterated and reinforced. The
patient was recalled after one week, one month
and three months for follow-up. [Fig 10] The patient
was comfortable and had gotten accustomed to the
rehabilitated stomatognathic system. Oral hygiene
instructions were reiterated and reinforced. On
completion of the treatment, the masticatory
efficiency was improved and esthetics also was
enhanced in harmony with the temporomandibular
joint. After a follow up of one year, the patient was satisfied with the outcome of the treatment and was
gratified with the enhanced esthetics and function.
Amelogenesis imperfecta is a genetic condition
that causes mottling of enamel in both primary
and permanent dentitions. This condition leads
to crippled appearance and deprived function of
the masticatory system. The permanent solution to revitalise the teeth would be to rebuild them using
the various philosophies of full mouth rehabilitation
laid down by several authors.
The routinely followed techniques are the Pankey-Mann-Schyuler (PMS) and Hobo’s technique.
Schyuler proposed the concept of “Freedom in
Centric”8
and in 1960, Pankey and Mann advocated
an organised sequential approach to full mouth
rehabilitation based on the principles of occlusion
advocated by Schuyler. Hobo adopted the concept
of posterior disclusion and gave the Twin-tables
Technique. The Twin-Stage Procedure was
developed as the advanced version of the Twin-Table technique. Youdelis scheme is advocated
for advanced periodontitis cases and for extremely
advanced cases of periodontitis Nyman and Lindhe
scheme is employed.9
All these philosophies have
deep rooted concepts and fundamentals upon
which occlusal rehabilitation is carried upon.
However, it is the clinician’s discretion to choose
an appropriate occlusal scheme for a particular
reconstruction case after a holistic review of the
presenting clinical condition so as to intertwine
predictable results with a stable functional
occlusion.
The present case, occlusal rehabilitation was
carried out using Pankey-Mann-Schyuler [PMS]
concept. The anterior guidance was established
first followed by rehabilitation of the mandibular
posteriors and finally the maxillary posteriors.7,10
Restoring the anterior teeth serves as a precursor to
achieve functional and aesthetically viable anterior
guidance. Anterior guidance is the dynamic
relationship of the lower anterior teeth against the
lingual slopes of the upper anterior teeth through
all ranges of function. Anterior guidance forms the
anterior control to provide posterior disclusion.11
The three main things that were taken care of
while replacing posterior teeth viz establishing the
plane of occlusion, achieving posterior disclusion
and deciding the type of occlusal scheme. PMS
concept endorses the development of group
function occlusion which has been incorporated in the patient as well. Functionally generated
pathway technique (FGP) was employed to achieve
group function occlusion. The plane of occlusion
was developed in tandem with the Curve of Spee
and Curve of Monsoon. Broadricks Occlusal Plane
Analyser was used for this purpose.
PMS technique allows stepwise sequential
restoration of teeth. The significance of that is the
treatment outcome can be envisaged even before
preparing any teeth in the patient. This philosophy
breaks down the complex treatment procedures
into fathomable quantum. The other advantages
of PMS technique include freedom in creating
desired occlusal plane, occlusal scheme and
intercuspation, creating and controlling porcelain
esthetics, teeth are prepared one quadrant/
segment at a time, chairside temporary restorations
can be constructed by quadrant or segment, final
impressions involve few teeth per impression. It
eliminates the chances of alterations to the vertical
dimension established since teeth are prepared
and restored in segmented simultaneous and
phased manner.12
The utilisation of PMS technique in this patient was
a deliberate choice considering its merits and the
patient factors. Simultaneous preparation of all
teeth for reconstruction could have jeopardised
the established vertical dimension. Since the teeth
were brittle due to genetic condition, a conscious
choice was made to adopt PMS technique over
others. The patient reaped maximum benefits from
this in the form of a well laid out treatment protocol
and reduced appointment length. Also, sufficient
gap between each appointment provided adequate
time for the patient to adapt and make corrections
to the prosthesis if required. The temporaries made
were ensured to be devoid of any discrepancies
and only after sufficient evaluation, they were
converted to permanent restoration. Porcelain
fused to metal restorations were used for all the
teeth and subgingival margins with appropriate
shade matching were done to achieve superlative
esthetic results. The definitive restorations were adjusted to remove any interferences in centric
and eccentric movements to incorporate group
function occlusion
The patient was reiterated about instructions
regarding proper oral hygiene measures and
reinforced to adhere to strict maintenance protocol.
Regular follow-ups were conducted and the
restorations were assessed to ensure optimum
oral health and function. Patient was elated and
satisfied at the end of receiving the prostheses
and adhered to the maintenance protocol.
The crucial elements to a successful treatment
outcome in full mouth rehabilitation for a patient
are meticulous planning and thorough fathoming
of the procedural steps. A well-established
anterior guidance synchronous to functional jaw
movements must be ensured to garner maximum
benefits and comfort. A detailed diagnosis and
treatment plan help to deduce and fragment
the complex procedures into simpler ones and
provides predictable success. Pankey-Mann
Schuyler philosophy, is the least cumbersome
and unequivocal concept that can be adhered to
restore normal function of a debilitated masticatory
system. This case report highlights the pertinence
of a full mouth rehabilitation technique as an
effective and efficient strategem in expediting
restoration of a mutilated dentition due to genetic
conditions.