3D printing is a revolutionary concept based on
additive process. It offers multifaceted applications
for dentistry in general and prosthodontics
in particular. A myriad of advantages like
reproducibility, accuracy, customisation and ability
to create complex parts with ease in less time have
provided improved patient treatment options and
compliance. This article presents an overview on
currently available technologies and their utilisation.
Abbreviations: CAD-computer aided designing,
FDM-fused deposition modelling, SLS-selective
laser sintering, SLA- standard triangular language,
PLA-polylactic acid.
Key words: 3D printing, CAD/CAM, additive manufacturing, bio printing, selective laser sintering, fused deposition modelling.
Charles Hull in 1983 printed the first 3D-object
using stereolithography.1
Digital dentistry was
pioneered by Francois Duret in 1970, with some
initial hiccups it took time to be integrated into
current practice.
Last few years have seen strikingly increased
application of 3D printing. The desired object/site
is scanned using an intraoral (IS) 3D scanner or
built using a CAD software. IS consists of a mini camera, integrated software and a computer.
Data is obtained as STF files (standard triangular
language)/STL (standard tessalation lan-guage).
This information is always broken down and stored
as triangles or tessellation. The tessellation is
the process of linking the surface with geometric
shapes to avoid overlaps and gaps. Stitching the
triangular files leads to a process of STL2
. These
STL files store the surface geometry of objects and
this information is encoded in ASCII (American
Standard Code For Information Interchange) or
Binary coding mostly which is used for small sizes3
.
This in-formation is used to print objects in layers
through various digital slicing and physically
re-produces layers with an automated process4
.
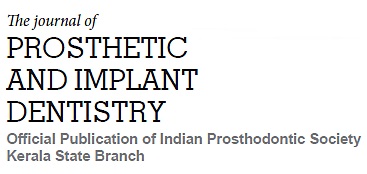
Additive Manufacturing is an additive process
referred to as rapid prototyping where a lot of
layers are added in contrast to traditional process
like subtractive manufacturing5
.
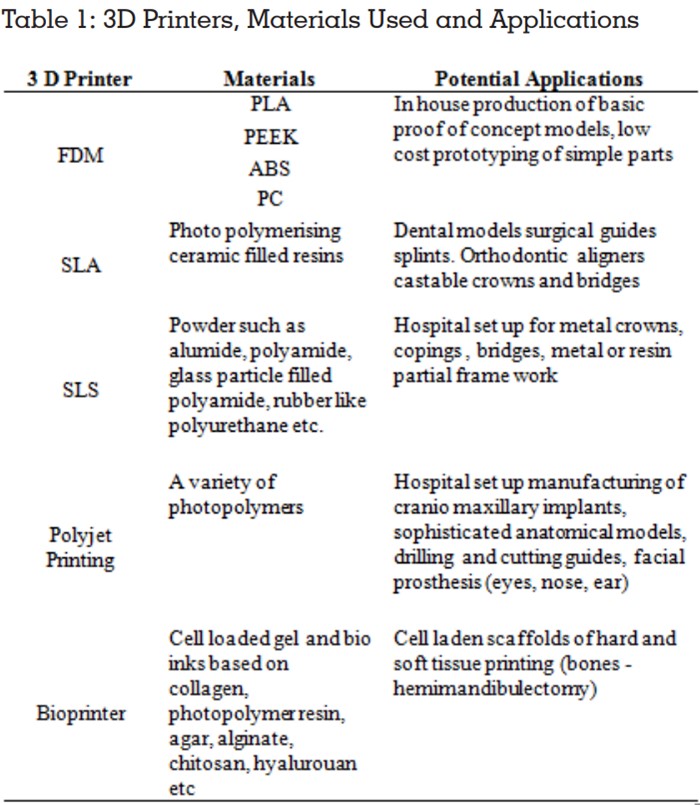
The most widely used additive methods include
fused deposition modelling (FDM), Stereo
lithography (SLA), Selective laser printing (SLS),
Polyjet Printing and Bioprinting6
, Direct metal laser
sintering. A variety of materials can be used which
include plastics, ceramics, resins and metals
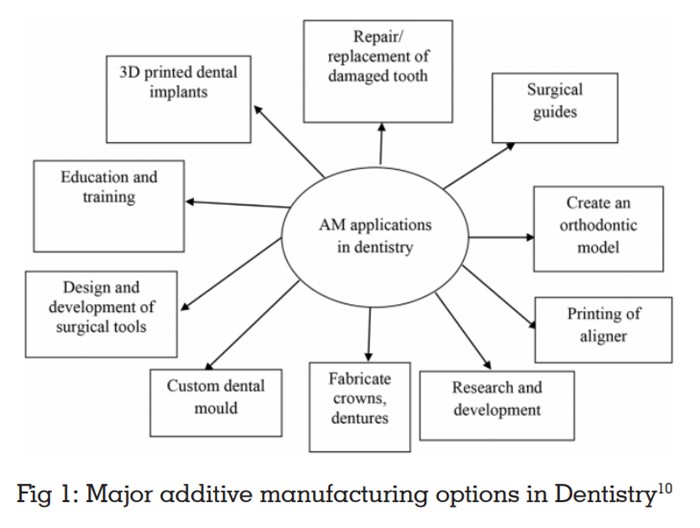
Developed by Scott Crump 1988, melted material
generally thermoplastic polymers such as poly
lactic acid (PLA) polycarbonate, polyether ether ketone (PEEK) is extruded through a nozzle to
print layer by layer. Print head has multi nozzle
and extrudes different types of material at the
same time7
. It is the printer of choice for in-house
production of 3D models8
. It is a flexible method
however its use is limited to temporary crown and
bridges manufacturing. Limitations include limited
colour selection, moderate printing resolution, and
complete removal of support material, surface
quality and time efficiency.
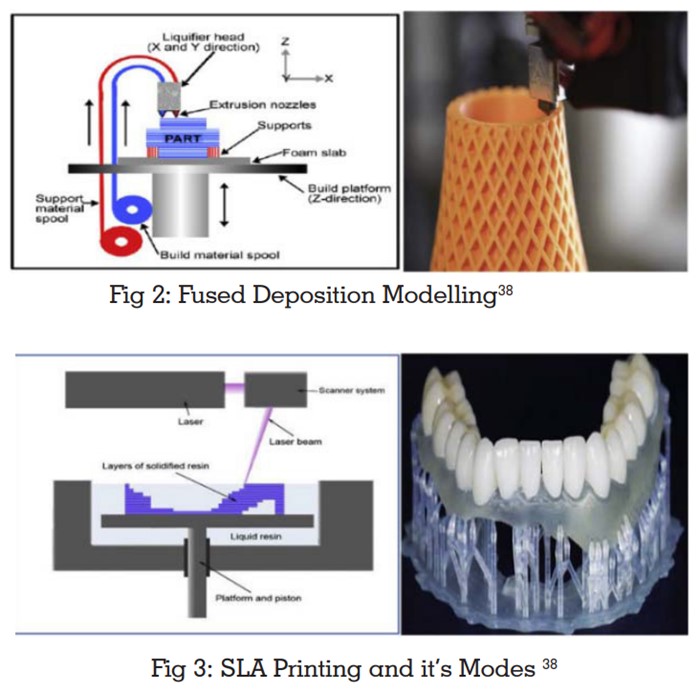
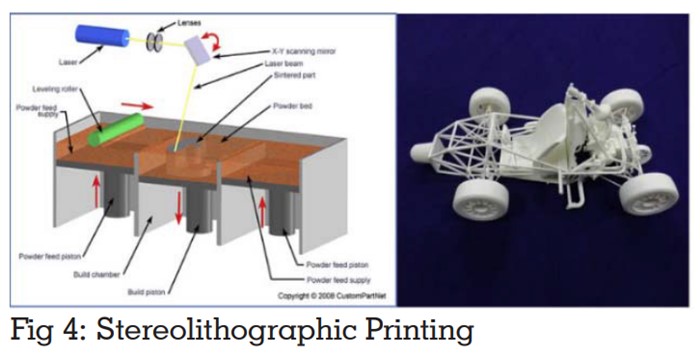
Both use laser to scan and build object layer by
layer but in selective laser sintering powder-based
material is used for printing.
SLA uses photo polymerisation - a process by which
the UV laser beam causes chain of molecules to
link together and form polymers.9
Products are built
with application of UV laser inside a vat of resin.10
SLA is used for printing from CT (DICOM data).
Advantages include good printing resolution as
compared to FDM; support material removal is
less too hence less wastage.
SLA is used to print surgical guides, aligners,
dental models and crowns, RPD’s, fabrication of
implant surgical guides.
SLS prints FDP’S, metal crowns and RPD’S. They
can replicate intricate geometries and provide
biodegradable scaffold for tissue engineering.
Printers with highest resolution. 3D model is
created one layer at a time by the printer head
getting layers of liquid photopolymer acrylic plastic
build tray followed by UV light curing11. It uses
widest choice of printing materials with varieties
in density, hardness, flexibility and porosity.
Resolution is as fine as 25-80 microns, faster
printing and replication of complex geometries.
Disadvantage includes post print model processing
such as intensive washing and removal of support
material.12
Applications include planning patient specific
3D models with complicated geometries, surgical
stents and guides, phantoms for orthopaedic
and cardiac surgeries, scaffolds for tissue
engineering.13, 14, 15
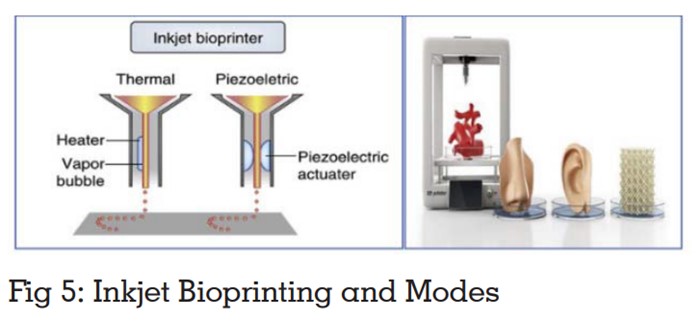
Uses photo polymerising materials stimulating natural cells such as chitosan, agar, alginate to
print hard and soft tissue scaffolds. Bio printing
uses cell ink based bio printers or spheroid or
micro tissue based systems have been developed
to generate artificial tissues, complex 3D in vitro
models.16,17 With that the additive manufacturing
has given a new face to discipline of stem
cell therapeutics with the flexibility of printing
cells into desired 3D complex, employing it for
transplantation and regeneration.18 3D printing
has found its applications in generating optimal
values of human bone and skin grafts in vitro.19
This has immense potential to replace the current
strategies of procuring auto grafts which is
associated with donor site morbidity and loss of
structure.20
This technology is used to produce metal parts with
high accuracy and better mechanical strength. In
this technology metal material is added layer by
layer and a laser beam is used to fuse metal at a
point.21,22 This uses titanium, cobalt, aluminium,
bronze alloy, steel. Approximate accuracy is 25-
35µm.
3D models are fabricated by adding layers of the
defined sheet of materials. A laser is used to cut
sheet as per the required cross section. Adhesives
are used to combine the layers and generated by repeating the steps.23,24
Powerful electron beam is used to build product
layer by layer by using a metal powder by
command of the CAD model with exact geometry.
Under a vacuum the raw material is stored and
fused by an electron beam.25, 26 Vacuum eliminates
impurities.
A literature search using search engines such as
Google scholar and Pubmed with keywords was
done, all articles from 2016 to 2020 printed in
English, inclusive of case reports, in vitro studies
and systematic reviews were considered.
Minev R, Minev E, 201627 stated that shrinkage
of 3D printed models is an unavoidable problem
during the printing process and it affects printing
accuracy of most 3D printers. FDM shrinkage
occurs due to thermal contraction when melted
filaments solidify. In SLA and multijet shrinkage
occurs due to polymerisation. Hambali RH, Cheong
KM, Azizan N, 201728 concluded that FDM has
bad surface quality due to staircase effect of
manufacturing using material extruding through
a nozzle. This was improved by approximately
97.2% via immersion in acetone solution for 300
seconds. This chemical treatment is one of the most
economical and fast methods to enhance surface quality of additive manufacturing parts for future
manufacturing industry. Raymond E Rebong et
al 201829 assessed the dimensional accuracy of
3D models with each other and compared with
traditional plaster casts. They concluded amongst
FDM, SLA, and Polyjet printing, the FDM had
fewest dimensional measurement differences as
compared to plaster mode.
Daniel Khorsandi et al 201830
Compared SLA and FDM methods of rapid
prototyping. They stated that SLA offers greater
efficiency, high level of accuracy. Layer thickness
of two different techniques FDM 0.5-0.127mm as
compared to SLA 0.05-0. 015mm. Both however
make rough patterns that need to be polished
to limit bacterial retention. Ucar et al, 201831
published an in vitro study to show that the
ceramics manufactured by stereolithography
show comparable mechanical properties to
milled ceramics. However, manufacturing process
and strength, fracture toughness are areas that require further research. To improve the properties
of ceramics so produced, porosity should be
eradicated resulting in denser more compact
mixture. Kim et al, 201832 proposed a new digital
prosthesis using an FDM printer to make a flask
for making a complete denture. This took 7 hours
to complete and showed satisfactory results in
terms of completeness of complete denture.
Using a universal development system software,
denture design STL and a denture flask STL were
superimposed, and the denture region was set as
an empty space. Conventional artificial teeth were
inserted into the 3D manufactured flask, resin
packing, finishing and polishing was done using
conventional method of fabrication of complete
denture. Fusong Yuan, Yao Sun, Lei Zhang, 201933
implant guide CAD and FDM 3D printing were used
to achieve a chair- side high efficiency design for
production of implant guides. Visual inspection
revealed that the positioning of 30 implant guides
was successful and retention was satisfactory. A
comparison of 3D data of printed implant guide
and CAD guide demonstrated a morphological
error of 0.5999 plus minus 0.146. Making FDM and
CAD time saving, efficient chair side methods. Lee
D et al, 202034 stated digital light processing 3D
printers (DLP) produce shrinkage depending on
the material and polymerisation method. Owing to
material characteristics the FDM accuracy of full
arch dental models is supposed to be higher than
that of the DLP however due to surface roughness
of the FDM method the crown preparation die for
dental prosthesis is not accurate. Therefore, a
new hybrid dental model that combines the FDM
for full arch and DLP for specific die is proposed.
Yoshiki Ishida et al, 202035 Compared the accuracy
of cylindrical patterns fabricated with consumer
FDM 3D printers with consumer SLA 3D Printers.
After the patency of FDM device expired, several
types of small consumer 3D printers were
introduced for personal use. The accuracy of
these less priced printers was compared with
dental FDM 3D and SLA 3D printers. The consumer
printers had worse accuracy than dental printers. An enlargement adjustment of 1-3% along the
horizontal axis was necessary to realise the set
design. In terms of surface roughness consumer
SLA produced smooth patterns. Hence, they
concluded that consumer printers have potential
to be used in dental applications.
Not only for manufacturing 3D has led to an
exemplary shift in training by providing idealistic
plastic typodonts to more real-life 3D printed
models that are based on data obtained by
intraoral scan of patients36. Polyjet printing has
successfully been used to create models in different
levels of hardness, replicating that of healthy
enamel, dentin and caries so that the trainee
experience proprioception of working on real
tooth37. 3D manufacturing undoubtedly offers a
promising future due to its multiple applications
and accurate detail reproduction however at the
same time it involves high investment cost. One of
its largest limitation is the quality. Due to the way
successive layers are deposited on top of each
other an inherent weakness is literally build into the
design. Finishing of final product is time consuming
and requires skill. Depending on the material
it may need additional treatment to reach full
strength. For example, zirconia blocks used require
further sintering to reach high strength. SLA can
be done only by using photopolymerising resins.
These are messy and can cause inflammation
and irritation on inhalation. Also, resins cannot
be heat sterilised.
3D printing has the potential of revolutionising
dentistry in general and Prosthodontics in
particular. Although the initial investment is high
and it requires training in usage, it helps to reduce the time for actual patient care. In today’s
scenario of emerging infective pandemics minimal
exposure to the clinician, technician and patient
can be offered. It can allow patient care from any
part of the world by exchange of information. It
has a great potential in research and treatment
modalities. Because the print object is produced according to the image of the patient, the print
can be tailored to optimally fit the condition of the
patient. The problem that requires further research
is the limitation of available material assortment
in particular when moving beyond the canonical
polymers as well as improvement of printing speed
and post processing requires.
Although it is not a replacement for conventional
treatment methods but its scope to improve and
develop is what the future of dentistry holds.
Source of support:
None.
Conflicts of interest:
The authors declare no
conflicts of interest.