Amelogenesis imperfecta is a congenital disorder which affects deposition, calcification and/or maturation of dental enamel. This genetic disorder affects teeth in both deciduous and succedaneous dentition leading to functional as well as esthetic in adequacies. This condition exerts radical reper-cussions on stomatognathicsyste mandintangible effects on the confidence of the patient. This clinical report elaborates on the multidisciplinary approach adopted for full mouth rehabilitation of a dentition affected by this genetic disorder in young adult patient. The treatment plan aimed at upheaving esthetics, restoring the vertical dimension and re-instating the masticatory function. Pankey–Mann– Schuyler philosophy of full mouth rehabilitation was adhered to achieve these treatment objectives. Full mouth rehabilitation albeit restoring esthetics and functional so imparts a substantial positive psychological upliftment and therefore revamps the patient confidence.
Key words: Amelogenesis Imperfecta, Full Mouth rehabilitation, Pankey-Mann-Schyuler philosophy, Broadricks Occlusal Plane Analyser
Amelogenesis imperfecta has been described as
a complex group of genetic disorder that primarily affects the enamel structure and exists independent of any related systemic disorder.1–2 Both
deciduous and permanent dentitions are affected
by this enamel anomaly.3
It is entirely ectodermal,
and the mesodermal components of the teeth are
unaffected. Amelogenesis imperfecta trait can be
transmitted either by autosomal dominant, autosomal recessive or X-linked mode of inheritance.
It is caused by mutation or altered expression of
genes such as: enamelin, ameloblastin, tuftelin,
MMP-20, and kallikrein.2
Amelogenesis imperfecta [AI] can be broadly
classified into four primary groups based on phenotype—hypoplastic, hypomaturation, hypocalcified and hypomaturation-hypoplastic. However, at
least fifteen subsets of amelogenesis imperfecta
have been identified when phenotype and mode
of inheritance are considered3
. Clinical findings
of AIinclude, enamel deficiencies, root malformations, impaired tooth eruption, pulpal calcifications, impaction of permanent teeth, progressive root and crown resorption, congenitally missing
teeth and tooth sensitivity. Since enamel thickness
is severely affected, teeth are undersized with
prominent spaces between the adjacent teeth,
compromised oral hygiene and mouth breathing
with associated gingivitis, gingival hyperplasia
and other periodontal problems. Other clinical
findings associated with amelogenesis imperfecta
include congenitally anodontia, open occlusal
relationship, multiple impacted teeth and taurodontism.4
Management of amelogenesis imperfecta is quite
challenging and arduous to accomplish. Comprehensive treatment planning shouldn’t be undermined and the critical procedure in the treatment
planning is the evaluation of vertical dimension
using mounted diagnostic casts and a diagnostic
wax-up. Age of the patient, type and severity of
the disorder, socioeconomic status and intraoral
condition at the time of treatment planning are
some of the influential factors that impact the
treatment planning in such patients. The final
objective of the treatment plan should be to weave
esthetics, masticatory function and general oral
health into harmony.
The rehabilitation of entire dentition for patients
with amelogenesis imperfecta can be achieved
successfully by using the philosophies of full mouth
rehabilitation. They provide tangible and everlasting esthetic result in tandem with occlusal harmony.
Full mouth rehabilitation procedures are a complex
set of procedures which restore the teeth to their
natural form, function, and enhances esthetics in
harmony with the temporomandibular joint and
the associated hard and soft tissues.5-6
Although several philosophies and protocols have
been widely documented, two of them are routinely
employed. They are, Hobo’s twin stage technique
and Pankey-Mann-Schuyler (PMS) technique. This
clinical case report illustrates the treatment procedures carried out sequentially in a full mouth rehabilitation using porcelain fused to metal crowns strictly adhering to Pankey– Mann–Schuyler philosophy in a patient with dilapidated dentition
due to amelogenesis imperfecta.
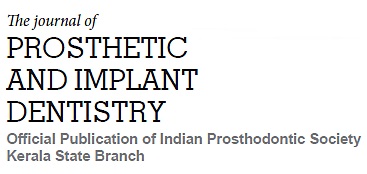
A 22-year-old female patient reported to the Department of Prosthodontics with a chief complaint of
generalized discolouration & stained appearance
of her teeth. She also expressed concerns regarding her teeth size, shape and shade along with
poor masticatory efficiency [Fig 1]. The patient had
no history of any major systemic illnesses. Clinical and radiographic examination of the patient
revealed no abnormality in temporomandibular
joint movements, generalized mild attrition and
discoloured teeth with irregular pattern of mineralisation. The patient did not have any loss of vertical
dimension of occlusion. Based on the clinical and
radiographic findings, the patient was diagnosed
with amelogenesis imperfecta and the patient was
advocated for full mouth rehabilitation to address
her chief complaint.
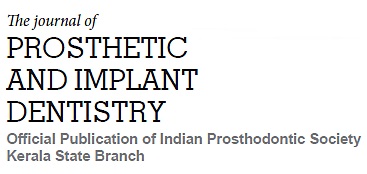
Preliminary impression of maxillary and mandibular arch was made using irreversible hydrocolloid and diagnostic casts were mounted on a
semi-adjustable articulator using interocclusal
record after a facebow transfer. Protrusive record was obtained from the patient to program
the articulator. Preliminary analysis was carried
out on the mounted casts followed by diagnostic
wax-up without altering the vertical dimension
was performed on the maxillary and mandibular
anterior teeth [Figure 2].
After preparing the maxillary and mandibular
anterior teeth [Figure 3] the provisional crowns
which were fabricated using the putty index of the
diagnostic wax‑up were luted using a provisional
cement. The provisional restorations given to the
patient were utilised to assess the anterior esthetics
and help determine the anterior guidance for the
patient. Once the patient got accustomed to the
established anterior guidance, a custom incisal guide table was fabricated on the articulator [Figure 4]. The final restorations for the maxillary and
mandibular anterior teeth were fabricated and
cemented after metal try-in procedure [Figures 5].
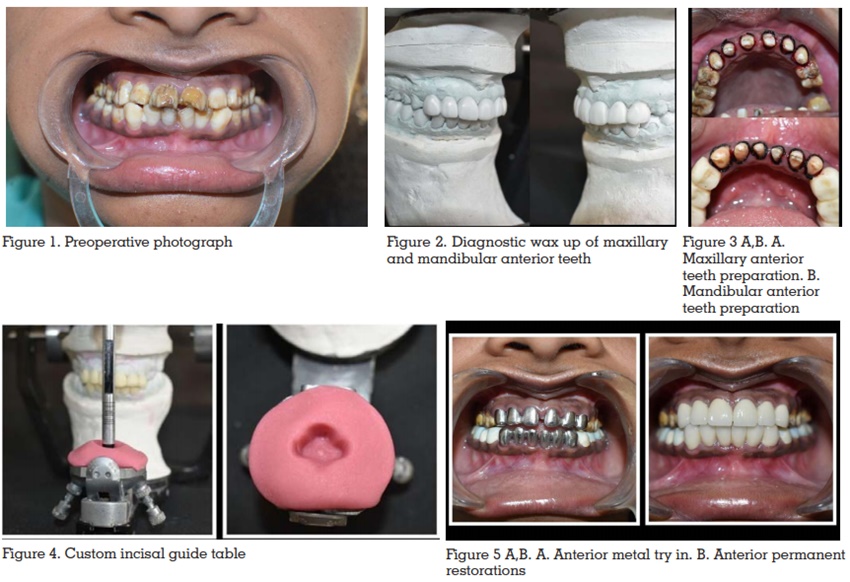
The subsequent procedure was to restore the
mandibular posterior teeth. Diagnostic wax-up
of mandibular posterior teeth was performed on
the mounted cast prior to preparation of teeth in
the patient. The occlusal plane and Curve of Spee
were established by using Broadricks Occlusal
Plane Analyser [Figures 6]. Then, to fabricate the
provisional restorations, putty index of the waxup was made. The temporary crowns fabricated
were cemented provisionally after teeth preparation. Tooth preparation and provisionalization
of mandibular posterior teeth were completed
segmentally.7
Patient’s occlusion and comfort were
evaluated for the next three weeks. When provisional restorations were considered acceptable, they were used to develop form and contour of
definitive restorations for the mandibular posterior
teeth. The final restorations of the mandibular
posterior teeth were cemented and succeeded by
the fabrication of maxillary posterior restorations
using the functionally generated pathway [FGP]
technique.
The maxillary posterior teeth were prepared [Figure 7] and a final impression was made to obtain
the maxillary master cast. Centric relation record
was made and utilised to mount the maxillary and
mandibular casts to the articulator. The patient
was asked to perform the centric and eccentric
movements which were recorded using functional
wax. This provided the FGP record. Quick setting plaster was poured into this record to obtain
the functional core index which was articulated
against the maxillary mastercast [Figure 8] to
develop the wax patterns for maxillary crowns in group function occlusion. After a bisque trial,
final restorations were luted and group function
occlusion was achieved. [Figure 9]
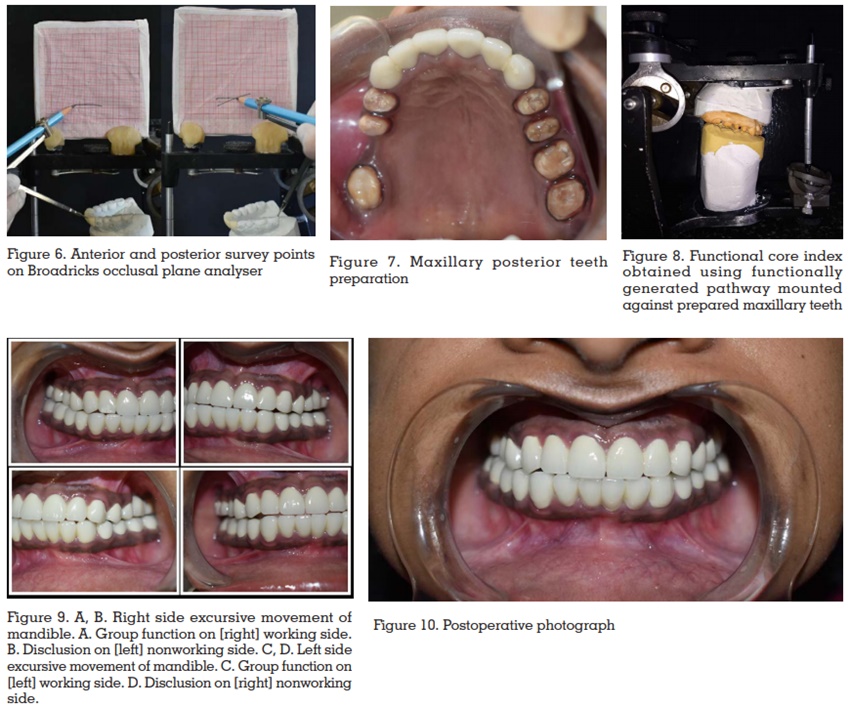
Regular recall and review protocol were effectively
employed and oral hygiene maintenance instructions were reiterated and reinforced. The patient
was recalled after one week, one month and three
months for follow-up. [Figure 10] The patient was
comfortable and had gotten accustomed to the
rehabilitated stomatognathic system. Oral hygiene instructions were reiterated and reinforced.
On completion of the treatment, the masticatory efficiency was improved and esthetics also was
enhanced in harmony with the temporomandibular joint. After a follow up of one year, the patient
was satisfied with the outcome of the treatment
and was gratified with the enhanced esthetics
and function.
Amelogenesis imperfecta is a genetic condition
that causes mottling of enamel in both primary
and permanent dentitions. This condition leads
to crippled appearance and deprived function of the masticatory system. The permanent solution to
revitalise the teeth would be to rebuild them using
the various philosophies of full mouth rehabilitation laid down by several authors.
The routinely followed techniques are the Pankey-Mann-Schyuler (PMS) and Hobo’s technique.
Schyuler proposed the concept of “Freedomin
Centric”8
and in 1960, Pankeyand Mann advocated an organised sequential approach to full
mouth rehabilitation based on the principles of
occlusion advocated by Schuyler. Hobo adopted
the concept of posterior disclusion and gave the
Twin-tables Technique. The Twin-Stage Procedure
was developed as the advanced version of the Twin-Table technique. Youdelis scheme is advocated for
advanced periodontitis cases and for extremely
advanced cases of periodontitis Nyman and Lindhe
scheme is employed.9
All these philosophies have
deep rooted concepts and fundamentals upon
which occlusal rehabilitation is carried upon.
However, it is the clinician’s discretion to choose
an appropriate occlusal scheme for a particular
reconstruction case after a holistic review of the
presenting clinical condition so as to intertwine
predictable results with a stable functional occlusion.
The present case, occlusal rehabilitation was
carried out using Pankey-Mann-Schyuler [PMS]
concept. The anterior guidance was established
first followed by rehabilitation of the mandibular
posteriors and finally the maxillary posteriors.7,10
Restoring the anterior teeth serves as a precursor
to achieve functional and aesthetically viable anterior guidance. Anterior guidance is the dynamic
relationship of the lower anterior teeth against the
lingual slopes of the upper anterior teeth through
all ranges of function. Anterior guidance forms the
anterior control to provide posterior disclusion.11
The three main things that were taken care of
while replacing posterior teeth viz establishing the
plane of occlusion, achieving posterior disclusion
and deciding the type of occlusal scheme. PMS
concept endorses the development of group function occlusion which has been incorporated in the patient as well. Functionally generated pathway
technique (FGP) was employed to achieve group
function occlusion. The plane of occlusion was
developed in tandem with the Curve of Spee and
Curve of Monsoon. Broadricks Occlusal Plane
Analyser was used for this purpose.
PMS technique allows step wise sequential restoration of teeth. The significance of that is the
treatment outcome can be envisaged even before
preparing any teeth in the patient. This philosophy
breaks down the complex treatment procedures
into fathomable quantum. The other advantages
of PMS technique include free domincreating
desired occlusal plane, occlusal scheme and intercuspation, creating and controlling porcelain
esthetics, teeth are prepare done quadrant/segment at a time, chair side temporary restorations
can be constructed by quadrant or segment, final
impressions involve few teeth per impression. It
eliminates the chances of alterations to the vertical
dimension established since teeth are prepared
and restored in segmented simultaneous and
phased manner.12
The utilisation of PMS technique in this patient was
a deliberate choice considering its merits and the
patient factors. Simultaneous preparation of all
teeth for reconstruction could have jeopardised
the established vertical dimension. Since the teeth
were brittle due to genetic condition, a conscious
choice was made to adopt PMS technique over
others. The patient reaped maximum benefits from
this in the form of a well laid out treatment protocol
and reduced appointment length. Also, sufficient
gap between each appointment provided adequate
time for the patient to adapt and make corrections
to the prosthesis if required. The temporaries made
were ensured to be devoid of any discrepancies
and only after sufficient evaluation, they were
converted to permanent restoration. Porcelain
fused to metal restorations were used for all the
teeth and subgingival margins with appropriate
shade matching were done to achieve superlative
esthetic results. The definitive restorations were
adjusted to remove any interferences in centric and eccentric movements to incorporate group
function occlusion
The patient was reiterated about instructions
regarding proper oral hygiene measures and
reinforced to adhere to strict maintenance protocol. Regular follow-ups were conducted and the
restorations were assessed to ensure optimum
oral health and function. Patient was elated and
satisfied at the end of receiving the prostheses
and adhered to the maintenance protocol.
The crucial elements to a successful treatment
outcome in full mouth rehabilitation for a patient
are meticulous planning and thorough fathoming of the procedural steps. A well-established
anterior guidance synchronous to functional jaw
movements must be ensured to garner maximum
benefits and comfort. A detailed diagnosis and
treatment plan help to deduce and fragment the
complex procedures into simpler ones and provides
predictable success. Pankey- Mann Schuyler philosophy, is the least cumbersome and unequivocal
concept that can be adhered to restore normal
function of a debilitated masticatory system. This
case report highlights the pertinence of a full
mouth rehabilitation technique as an effective
and efficient strategem in expediting restoration
of a mutilated dentition due to genetic conditions.