Glossectomy whether it is total or partial can result in significant functional impairments in mastication, swallowing, and speech. Voice quality and resonance are compromised because of changes in oral cavity volume, and articulation, management of food and protection of the airway are also jeopardized. Oral rehabilitation through prosthetic management can be very helpful in reducing these problems. Prosthetic rehabilitation can also improve the patient’s appearance and psychosocial adjustment. A broad search of published literature was performed using the keywords glossectomy, glossal prosthesis, Palatal augmentation and tongue prosthesis from 1958 to 2018 in Medline, Google scholar and internet. This article aims to review and give basic knowledge of various techniques that can be used in prosthetic rehabilitation of glossectomy patients in different clinical scenarios.
Key words: Glossectomy. Tongue prosthesis. Palatal augmentation prosthesis. Guiding flange. Articulation
The tongue is one among the most frequent site
for oral cancer. From a psychosocial point, it is
one of the most devastating tumor. Mode and
aggressiveness of treatment is determined by the
size, type and location of the tongue lesions. Even
then surgery with or without adjunctive therapy
remains the treatment of choice. In most cases
they are done in conjunction with radical neck
dissections, mandibulectomy, laryngectomy, or
other mutilating procedures.1
Loss of tongue results
in varying degrees of impairment of mastication,
deglutition, and speech regardless of the extent
of the surgical resection.2
Functional rehabilitation
in these patients can be attempted with a wide
variety of techniques and prostheses including
skin grafts, local and regional myocutaneous
flaps, dental prostheses, and prosthetic tongues.3
The feasibility of a prosthodontic approach to
treatment depends on the type and extent of
surgery. The primary concern of any rehabilitative
effort should be swallowing.1
Mandibular tongue
prosthesis is the treatment of choice in a total
glossectomy. A palatal maxillary prosthesis should
be considered in situations involving edentulous
patient undergone partial glossectomy and an
irradiated, resorbed mandibular ridge.4
This article
reviews different techniques that can be used in
prosthetic rehabilitation of glossectomy patients.
The ability to chew and swallow as well as the
production of elements for speech articulation
which involves tongue positioning is impaired in
total and partial glossectomy patients. Articulation
is affected because of the inability of the patient to
attain the proper cavity shapes and constrictions
necessary for precise sound production. Further
deterioration of oral function occurs if the mandible
is resected.5
The rehabilitation depends on the
extent of surgery. Functional rehabilitation can
be attempted with a wide array of techniques
and prostheses including skin grafts, local and
regional myocutaneous flaps, dental prostheses,
and prosthetic tongues.3
Before treatment, the
clinician should evaluate the mobility and sensory
status of remaining structures. These findings
should be correlated with swallowing studies,
patient expectations, and motivation to determine
realistic treatment goals.
The first objective of a prosthetic approach
to treatment was to determine a prosthesis
design that would increase the speaker’s
potential for constricting and occluding, that
is, shaping of the vocal tract, thereby achieving
a closer approximation to normal resonance
characteristics.6
Prosthesis might facilitate speech in the following
ways:
In addition to these features, a channel that is
located laterally in the prosthesis might enable
the patient to direct liquids and pureed foods
between the prosthesis and the lower alveolar
process, and into the oesophagus.7
There are various clinical scenarios which are
treated with different types of tongue prosthesis.
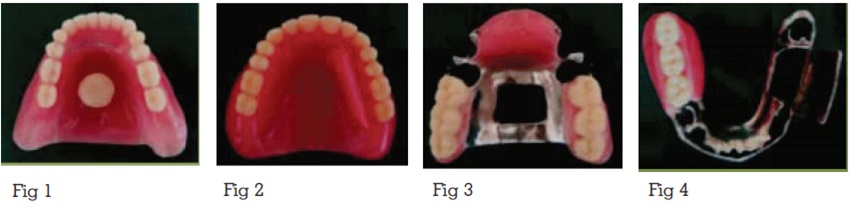
Treatment: Mandibular denture extending over
the floor of the mouth with a mushroom shaped
button attached to it on which silicon tongue can
be placed.
In this Impressions are made with irreversible
hydrocolloid material using a maxillary tray for
mandibular arch to record the floor of the mouth.
The floor of the mouth becomes concave after a
total glossectomy. The mandibular base extends
over the floor of the mouth. A “mushroom like”
button is constructed on the mandibular prosthesis
so that a silicone tongue can be snapped over it.5
It can also be attached to the first part by a flexible
“collar button” type attachment.8
Magnet can also
be used to attach silicone tongue component to
the acrylic resin base instead of the mushroom
like projection.4
Two prosthetic tongues can be made, one for
speech and one for swallowing. The tongue
made for speech is somewhat flat, with a slightly
wide anterior elevation to aid in articulation of
linguoalveolar sounds `t` and `d` and to aid
in shaping the oral cavity for improved vowel
production. The tongue for swallowing is made
with a trough in the posterior aspect to guide the
food bolus into the oropharynx.9
One of the objectives for the prosthetic tongue is
to increase the speaker’s potential for shaping the
voice tract to achieve closer to normal resonance.
The dome-shaped tongue fills the palatal vault,
anterior-to-posterior and laterally, much as the normal tongue when the mandible and teeth are
closed.3
By varying the vertical distance between
the palate and the prosthetic tongue surface,
the resonance characteristics of speech can be
changed. Vowels, such as /a/, /e/, and /u/, could
not be distinguished without the speech tongue.
Lingua-dental consonants (/th/) were substituted
with the lingua-alveolar consonants (/d/ and /t/).
The lingua-alveolar and lingua-velar (/g/ and
/k/) consonants are produced by anterior-to-posterior positional changes of the mandible in
the horizontal plane.6
Treatment:
1) Mandible is reconstructed with
bone graft and implants are placed. After that
implant retained overdenture is made with tongue
prosthesis.10
2) Mandibular complete denture obturating the
defect and maxillary complete denture with a
guiding flange.9
Loss of continuity of the mandible affects the
balance of the lower face. It leads to deviation of
the residual segment toward the resected side.
A guiding flange is made to limit the deviation of
mandible towards the resected side.5
In implant retained overdenture, use of dental
implants improves the biomechanical properties
of the prosthesis and assist in regaining some
masticatory function.10
It was also noted that ossseointegrated implants
can provide reliable retention for prosthesis in
edentulous patients but additional surgeries,
higher expense and prior radiation therapy might
contraindicate implant treatment.4
Treatment: Maxillary cast partial denture with palatal augmentation.
The palatal augmentation prosthesis is used
in glossectomy patients to restore impaired
speech and swallowing by artificially lowering
the palatal vault in order to provide contact
between the remaining tongue and the palatal
contours.9
A Dentulous patient treated with a
partial glossectomy and radiation therapy, in
the absence of a Mandibular resection, may have
difficulty with speech and swallowing. This may be
a result of loss of tissue in the region or of fibrosis
secondary to radiation therapy. The function of the
residual tongue is traced with softened modelling
compound. The patient is asked to repeat the
linguovelar sounds /k/ & /g/ for the posterior palatal
tracing and the linguoalveolar sounds/t/ & /d/ for
the anterior palatal tracing. The compound gets
moulded accordingly and then final tracing is
done with functional wax, and the entire traced
area is processed in clear acrylic resin.5
Modification
If acceptable speech articulation is attained for
most elements of speech except the linguoalveolar
fricatives `s` and `t`, another modification can be
done. A narrow, sharp groove carved in the midline
of the palatal prosthesis can, by directing the air
stream, improve the production of these sounds.5
The application of palatal augmentation prosthesis
might not improve the swallowing function
sufficiently in some patients for whom a large part
of the tongue has been resected and the range of
movement of the tongue is markedly restricted. In
these cases, both palatal augmentation prosthesis
and lingual augmentation prosthesis should be
used in patients with dysphagia after malignant
tongue tumor resection.11
Treatment: Mandibular cast partial denture obturating the defect with a guiding flange
and maxillary cast partial denture with palatal
augmentation. A cast metal Mandibular prosthesis
can be suggested for a patient lacking the motor
skills to bring the mandible into occlusion, when the
mandible can be manipulated into an acceptable
maxillomandibular relationship. The guidance
flange for the mandibular framework was designed
to extend on the non defect side. Thereby assisting
in controlling mandibular deviation and coordinate
masticatory movements for a patient following a
segmental mandibulectomy.12
Maxillary inclined plane prosthesis with cast
chrome cobalt framework can be also given in
case of subtotal glossectomy. It was also noted that
there was a negative change in speech resonance
because of a large prosthetic mass in the oral
cavity. But it was concluded that swallowing as
well as speech was substantially improved with
the use of prosthesis.2
Tongue is the major articulator during the
production of all phonemes except bilabial, labio-dentals and glottal sounds. Tongue movements
alter the shape of the oral cavity and change the
resonance characteristics that produce different
consonants. The coordination of the muscles and
nerve is impaired in glossectomy patients even
after reconstruction by flap.9
A properly fabricated Mandibular prosthesis or
a palatal augmentation prosthesis which is done
in a systematic manner with the assistance of a speech pathologist can achieve the following:
The functions of speech and deglutition are
achievable up to an extent without the tongue.
But it can be further enhanced towards normalcy
with the help of artificial tongue prosthesis.12
Early placement of prosthesis to obturate the large
defect created by a complete glossectomy improves
the patient’s ability to produce intelligible speech
and return to a relatively normal diet.13
Patients who have undergone partial glossectomy
are rehabilitated with palatal augmentation
prosthesis whereas those who have undergone
total glossectomy are rehabilitated with tongue
prosthesis for the Mandibular arch.14 But when
resected region is large and the tongue’s range
of movement is markedly restricted, in such cases,
lingual augmentation prosthesis is required along
with palatal augmentation prosthesis in order to
enhance the function of the remaining tongue and
swallowing. Palatal augmentation prosthesis aids
in contact between tongue and palate. But In these patients, when palatal augmentation prosthesis
alone is used, a functionally significant gap
develops between the tongue and the mandible
during swallowing.11
The extend of tissue loss determines the degree of
articulation impairments in glossectomy patients.15
Patients who had undergone total glossectomy
seemed to develop compensatory patterns of
speech, whereas patients who had undergone
partial glossectomy require prosthodontic treatment
and speech therapy to develop compensatory
articulation.16
The restricted motion of the tongue and lack of
lingual-palatal contact are the main causes of
speech impairment. Prosthesis can be functionally
formed to lower the palatal vault since contact
between the tongue and the posterior part of the
palate is anatomically impossible.17
In partial glossectomy cases, palatal vault can
be lowered by fabricating a false palate on the
maxillary hollow palate denture to enable the
tongue to function against it during speech.
During the fabrication of prosthesis, speech is often
used as a diagnostic tool in placing the anterior
teeth. Similarly, speech can be used to determine
the proper placement of a speech portion of the
prosthesis.4
For the successful function of prosthesis, Space
of Donders is essential. Space of Donders can be
described as the space between the dorsum of the
tongue and the hard palate when the mandible
is in rest position following the expiratory cycle
of respiration.18
The tongue and palatal augmentation prosthesis
created changes within the vocal tract resulting to
changes in the resonating system.10 A fixed tongue
prosthesis can help in certain ways to improve the
formation of consonants. Certain consonants like
“t,” “d,” etc., require contact of the tongue with the
palate. Although the artificial tongue is fixed, by
closure of the jaws it can be made to touch the
palate, with marked improvement in the formation of these consonants. Again, consonants like “c,”
“s,” etc., require a jet of air to be forced in between
the tongue and the palate. Here, also, the artificial
tongue can be elevated by closing the jaws to form
the cleft between the tongue and the palate through
which the jet of air can be forced out to form the
consonant.19 Speech therapy is also essential for
better functional outcome.14
Vowel intelligibility was improved in glossectomy
patients with the help of a prosthetic tongue. Placing
a groove in the lateral aspect of the prosthesis has
afforded a practical means of introducing most
liquids and pureed foods into the oesophagus.7
Interim palatal augmentation prosthesis can be
made by using a light-cured resin instead of using
techniques that include the use of incremental
additions of wax, modelling compound, or tissue-conditioning material to an acrylic resin base.20
While fabricating a tongue prosthesis, the dome-shaped speech tongue, with dimensions of contour
and bulk similar to a normal tongue, seemed to
be more functional design for both speech and
food management. Also it helps to strengthen the
Mandibular and oral musculature.9
It is easier to achieve more normal Mandibular
movements, masticatory performance and
improved appearance in dentulous patients
compared to edentulous patients.21
Consideration should be given to the patient’s
chief complaint when planning treatment for
glossectomy patients. Factors such as the extent
of the surgical resection, type of reconstruction, the
mobility of the residual oral and paraoral tissues,
neuromuscular coordination, mental proficiency,
and motivation should be kept in mind while
rehabilitating these patients.22
The paper reviews technical steps used for the
prosthetic rehabilitation of glossectomy patients.
The prosthetic tongue might not replace the intricately mobile structure of the tongue, which
is capable of infinite movements in swallowing
and speech.7
But the tongue prosthesis serves
the dual purposes of speech rehabilitation and
maintenance of good nutrition with oral feedings.2
Design of the prosthesis varies according to patient
needs. The prosthetic design for a total glossectomy
patient differs from a partial glossectomy patient.
So to improve the articulation, resonance and
food intake of a patient, a combined effort of
a maxillofacial prosthodontist and a speech
pathologist is essential. A well fabricated prosthesis
not only improves the function but also improves
the appearance and psychosocial well being of the
patient thereby helps in enhancing socialization.5