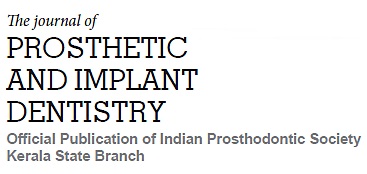
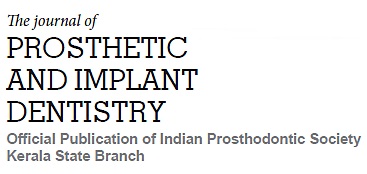
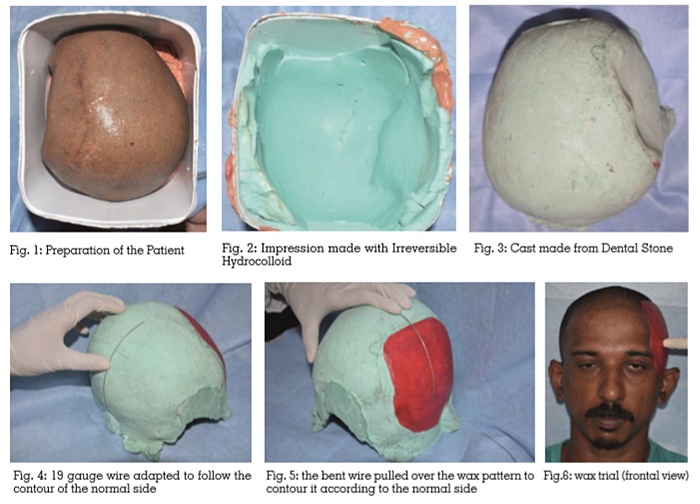
With advanced treatment options for treating head injuries and diseases of the brain, a large number of patients are reporting for cranial prostheses. Cranial prosthesis not only relieves pain and discomfort but also improves the psychological well-being of the patient. Smaller defects can be closed surgically. But larger defects require prosthesis mainly; implants. Titanium is the material of choice for the implant prosthesis. The prosthesis should be made precisely. It is usually made on or from a wax pattern. The case report describes an easy and inexpensive method of contouring the wax pattern. The wax pattern was made on a model and was contoured using a 19 gauge stainless steel wire. It was tried on the patient and then the implant prosthesis was fabricated.
Key words: Cranioplasty, Cranial Implant, Rehabilitation, Titanium Prosthesis.
Nowadays, rehabilitation of cranioplasty patients is becoming quite common. This may be due to the advances in the field of medicine that newer surgical techniques are used to treat patients with head injuries and other diseases affecting the brain.1, 2 Usually a portion of the skull or the cranium is removed as part of the treatment to avoid compression of the brain. Later, it becomes mandatory to use prosthesis or an implant to protect the underlying brain tissue and to improve esthetics3. Various techniques and biocompatible materials are available for esthetic reconstruction of the skull defect4. The following is a newer technique for the rehabilitation of such patients.
A thirty year old male patient reported as a reference from the Department of Neurosurgery for prosthetic rehabilitation of a cranial defect. The chief complaint of the patient was disfigurement. The patient had undergone craniectomy of the fractured fragments of frontal, temporal and parietal bones on the left side and a cranial implant made of Titanium was fabricated.
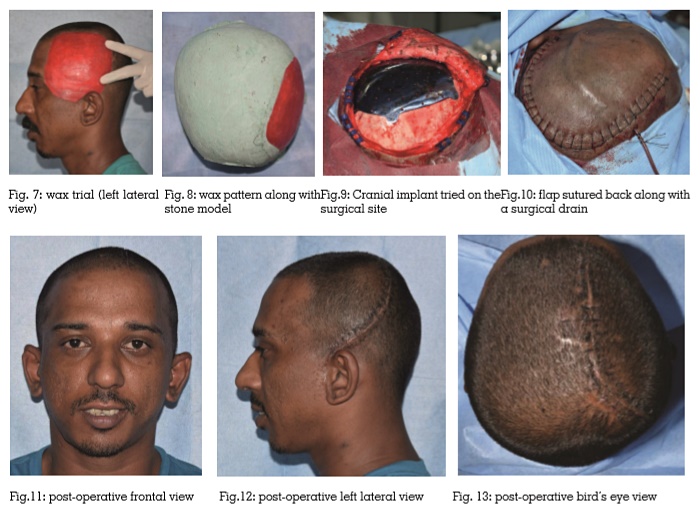
Trauma accounts for most of the cranial defects. During the repair of compound skull fractures or fractures penetrating the brain, removal of significant portions of the skull may be required. Successful restoration of these defects then demands prosthetic rehabilitation5. Pronounced cranial defects produce psychological trauma for the patients and consequently the patient refrains from carrying out their daily activities6. Also exertion and rapid movement can result in pain and discomfort. Some clinicians feel that the cranial implant “splints” the brain, decreases its mobility, and thereby relieves these symptoms5.
Small defects (2-3cm) located immediately above the orbital rim or nasion is probably reconstructed for esthetic reasons while restoration of large defects includes esthetic enhancement along with protection of the brain5. Reconstruction of the cranial defect can be taken up as a primary or secondary procedure depending upon the duration, severity of injury, location of the defect and condition of the overlying soft tissues. Immediate repair of cranial defects is discouraged by most clinicians4.
Osteoplastic reconstruction by the use of autografts from iliac crest, rib, tibia and calvarium, either as a free graft or transferred on a vascularized pedicle is a proposed method for repairing defects less than 5 cm in diameter. Although biocompatible and easily harvested, there is risk of resorption and loss of contour. Sometimes they can get infected and warrant removal. Allografts and xenografts have also been used but the outcomes attained are not very promising. Some of the alloplastic materials that may be used for such reconstruction include metal, acrylic resin, polyethylene and silicone4. Rehabilitation of larger defects is possible mostly with alloplastic materials. Fabrication of such prosthesis should be done with great care as it affects esthetics and function7,8.
The complexity in rehabilitating cranioplasty defect increases with increased defect size. It is difficult to produce a symmetric, accurate implant presurgically or at the time of surgery when the defect is greater than 50cm2 9. Many methods exist for the fabrication of presurgical customized cranioplastic implants, including the recently introduced medical imaging and three dimensional (3D) biomodeling. Here, the operation time may be reduced, but in cases of bilateral cranial defects and asymmetrical skulls, the mirrorimage process cannot be used10.
The described technique for the rehabilitation of a patient with a cranial defect using 19 gauge stainless steel wire for wax pattern contouring is a novel, easy and a less expensive method. Using this technique considerably decreases the number of patient appointments with lesser number of wax trials. The rounded edges of the stainless steel wire produce a smooth even surface finish for the wax pattern. The Prosthodontist is able to achieve a more accurate and predictable esthetic result in a limited time frame. The patient is not exposed to any radiation for the fabrication of the cranial implant. But this technique cannot be used in case of bilateral cranial defects.
Fabrication of the prosthesis for larger defects in cranium is usually made from wax pattern. The fabrication should be done with great care especially when it is in the esthetic zone. The above described technique is a novel and easy method for fabrication of wax pattern used for making titanium implant cranial prosthesis.