Alveolar ridge resorption is a biological phenomenon that occurs following tooth extraction. This review delivers an overview of recent advances in bone grafting materials and its benefits in ridge augmentation procedures. The biological performance of various grafting materials are reviewed based on clinical studies and animal studies. None of the bone grafts available today exhibits suitable biocompatibility, bioabsorption, osteoconduction and osteoinduction simultaneously. The choice of different bone substitutes may depend on the specific clinical situation and the restorative treatment plan. Currently available bone grafts provide mainly osteoconduction as a scaffold. Along with the availability of new technologies, use of newer bone grafts are emerging day by day. It is necessary to perform rigorous clinical studies of recently advancing bone graft materials to confirm their benefits and cost effectiveness in implant dentistry.
Implant treatment for the prosthetic rehabilitation of missing teeth is an advancing field of dentistry today. The common reasons for tooth loss are periodontal problems and tooth fracture.1 These may result in alveolar bone resorption compromising bone quantity, quality and morphology.2 Alveolar ridge resorption following tooth extraction varies with individual and plays a key role in the diagnosis and treatment planning of implant.3,4 The ultimate aim of the ridge augmentation is to replenish the hard tissues of the alveolar ridge and to simplify the prosthetic rehabilitation. So alveolar ridge augmentation is an unavoidable procedure for the longevity of the implant prosthesis.
Guided Bone Regeneration (GBR) is an advanced and predictable technique for alveolar ridge augmentation by the use of bone grafts5,6 and researches shows that it can generate an alveolar bone height in the range of 5.0mm- 8.5mm on average in severe defects.7-12
The bone graft materials can be categorised classically as autogenous bone, allografts, xenografts, and alloplasts.13 The properties of these biomaterials includes biocompatibility, space making capability, bio-absorbability and volume maintenance. The present review made an attempt to agglomerate knowledge regarding recent advances in the bone grafts, its use in implant dentistry and prosthetic reconstruction and to facilitate further advancements on bone grafts for future revolution for the success and prognosis of implants.
Generally graft materials can be classified as autografts, allografts, xenografts and alloplasts. Common properties of graft materials are osteogenic, osteoinductive or osteoconductive properties. Osteogenic property of the grafts enable them to differentiate into bone cells. The osteoinductive grafts stimulates the host mesenchymal cells to differentiate into osteoblasts that can form new bone. Osteoconductive grafts act as a three dimensional scaffold into which surrounding bone tissue can infiltrate and migrate through the lattice rather than induce bone formation. An illustration of classification of bone grafts is below (Table 1)
Bone grafts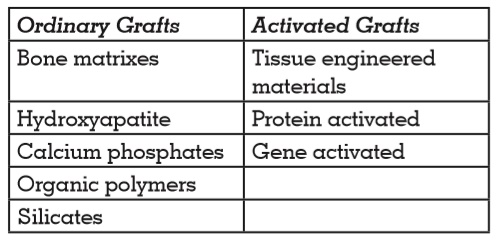
Autografts (Autogenous Bone)
Autografts are defined as the bone tissue harvested from, and implanted in the individual. These are considered as the “gold standard” in bone augmentation procedures because of its biocompatibility, osteogenic, osteoinductive and osteoconductive properties.14-16 The rationale for gold standard status is that only autogenous bone contain osteogenic cells within the bone matrix. Autografts can be cancellous, cortical, or cortico-cancellous and among these cancellous autogrfts are the preferred for augmentation of alveolus because of its rapid revascularisation and integration into the host site.17 Cortical autografts are composed of necrotic bone that provides an osteo-conductive character for bone formation that is why revascularisation and integration is very slow. Autogenous bone grafts can be harvested either from extra-oral or intra-oral sites to be used in block or particulate forms. Particulate autografts are obtained commonly from maxillary tuberosity, exostoses, and edentulous ridges and block grafts from rami and chin18. The extra-oral sites for autografts include the iliac crest, ribs and tibia. Though it is called as a “gold standard”, it has disadvantages such as donor site morbidity, additional surgical procedure to retrieve the bone, restrictions in the quality and quantity of bone, post-operative discomfort, and additional cost19. Autogenous graft can be used alone or in combination with other bone substitutes to form composite grafts20,21. According to histomorphometric studies eventhough autogenous bone exhibits faster initial bone formation at the receptor site, the final amount of bone formation did not differ from that reported with bone substitutes.22,23
Bone substitutes
Allografts, xenografts, and alloplasts together comprises bone substitutes. Bone substitutes should be biocompatible, biodegradable, nonantigenic, non-carcinogenic, inexpensive, noncontageous, bio-absorbable, able to regenerate, capable of space making and permit sufficient transport of gases, nutrients, and regulatory factors.24 Current bone substitutes induce only osteoconductivity as a scaffold and does not has osteoinductivity.
1. Allografts
Allografts are graft tissues obtained from and implanted into individuals of the same species.25 Allografts can be fresh frozen, freeze-dried or demineralized freeze dried materials. The cadaver bone is a good source of allograft and considered as an alternative for autograft due to its resemblance in the bone augmentation properties. Allografts can be obtained from cadaver or from the tissue banks. They are available in powder, cortical chips, cancellous cubes and cortical granules.25 They were subjected to various processing methods such as physical debridement, ultrasonic washing, ethanol treatment, and antibiotic wash before introducing into the bone augmentation site.26
Whittacker et al reported that allografts had both osteoinductive and osteoconductive properties but some other studies explained that allografts had only osteoinductive properties.27,28 The replacement of demineralised freeze dried bone allograft with vital bone is more pronounced than freeze dried bone allograft when grafted in extraction socket.29 Comparative studies of cortical and cancellous freeze dried bone allograft have shown that there was no significant difference in the final new bone formation at extraction sites.30 The disadvantages are increased risk of immunogenicity, quicker resorption rate compared to autogenous bone and a risk of disease transmission.
2. Xenografts
Xenografts are tissue grafts between two different species. The main sources of xenografts are deproteinized bovine bone matrix and porcine sources. Xenografts are indicated in periodontal infra-bony defects. Histological studies have claimed that infiltration of bovine xenograft particles with newly formed bone could fill the interparticulate space.31 Methods to reduce antigenicity of xenograft are similar to those used to process allografts.
3. Alloplast
These graft material are artificially derived and do not originate from humans or animals. Calcium phosphate materials are alloplastic grafts having similar mineral composition as that of bone. Hydroxyapatite, alpha tricalcium phosphate and beta tricalcium phosphate have been used as fillers during augmentation procedures or combined with autogenous bone as composite graft materials.32 They act as an osteoconductive scaffold for the osteogenic cells. The alloplastic grafting materials can be used in combination with bone promoting agents, exhibiting predictable bone augmentation in implant sites.
Activated bone grafts
Activated bone grafts can be categorised based on the nature of osteoinductive components as: 1) Tissue-engineered Bone Grafts, 2) Bone Grafts with Growth Factors, and 3) Gene- activated Bone Grafts.
Tissue-engineered bone grafts comprises two main components: a bio-resorbable scaffold and live cells. The mechanism of action of these grafts are concerned with the paracrine activity of cells of the graft.33 Ridge augmentation produced by the transplanted cells of tissue engineered bone graft is positively influenced by the osteogenic properties of Bone morphogenetic protein (BMP), vascular endothelial growth factor (VEGF), and stromal -derived factors (SDF-1).
Bone Graft with Growth factors consist of a scaffold and growth factors. Many growth factors have widely been tested in vivo models. Of these, Bone Morphogenic Proteins (BMPs) is important as they induce osteogenic precursor cells into osteogenic cells and have shown tremendous bone growth in many animal and also human clinical studies. Development of injectable formulations of BMPs with carriers are under research today. Examples for other growth factors besides BMPs includes platelet-derived growth factor(PDGF-BB), transforming growth factor-β, insulin-like growth factor-1, protein P-15, enamel matrix protein and fibroblast growth factor and so on.
The mechanism of bone augmentation by growth factors are by cell proliferation by mitosis, migration, differentiation and apoptos is as well. The TGF-β and the factors released by the bone matrix such as insulin (IGF-1 and 2), the fibroblast growth factor (FGF-2) and growth factor derived from platelets (PDGF) are potent mitogens which plays a key role in osteoblast proliferation. The drawbacks of bone grafts with growth factors are rapid biodegradation of protein molecules,which may lead to short life span of the graft and short duration of action of the graft due to limited amount of therapeutic protein at the recipient site of the graft.
Gene-activated Bone Graft A gene- activated bone substitute is a complex scaffold-nucleic acid combined using methods such as chemical binding, adjuvants or direct incorporation of nucleic acids into the scaffold at a certain stage of matrix synthesis.34-35 Pre-requisites associated with geneactivated material handling include: sterilization, standardization of control for preservation of the specific activity of the gene construction after the completion of production cycle, the necessity of the transfection level of nonviral gene constructions and their prolonged release from the scaffold’s structure after implantation.
Composite grafts
Sticky bone is a composite graft developed in the year 2010 and composed of a network of fibrin.36 Advantages of sticky bone are its ability of moldability, prevention of movement of grafted bone, growth factor release, minimization of in growth of soft tissues into the graft and it doesn’t require the need of biochemical additives for processing. Fabrication of sticky bone is easy and is an effective material for the reconstruction of edentulous alveolar bone defect, based on the concept of minimally invasiveness on ridge augmentation.
Barrier membranes
Implants treatment can be done as one stage surgery along with bone augmentation or following bone regeneration as 2 two stage surgery based on the amount of localized bone deficiency. Horizontal and vertical ridge augmentation procedures often require the use of autologous bone block graft combined with a membrane or a particulate autograft with a bone substitute and a membrane. BioMend, Periogen, Paroguide, BioGide, BioBar are some examples of commercially available collagen barrier membranes and among these BioGide having the longest duration of resorption period.
Various graft materials were histologically studied by Nappe et al to evaluate the characteristics, the percentage of bone formation and residual graft particles and reached a conclusion that there were differences in newly formed bone percentages between the allograft and the xenograft, whereas no significant differences of bone formation were found between the allograft and the alloplastic grafts and no significant differences in the percentage of residual particles amongst the different types of graft.37
Histologic and histomorphometric studies by Fadel R A et al for the evaluation of the bone regeneration in critical size calvarial defects in rats grafted with either a deproteinized bovine bone mineral alone or in combination with a single or double layer of native bilayer collagen membrane and the residual deproteinised bovine bone mineral in these defects demonstrated that guided bone regeneration needs resorbable collagen membranes for bone regeneration.38
1. Platelet –rich growth factor (PDGF)
Severalin-vitro and in-vivo studies regarding platelet rich growth factor demonstrated its ability to enhance the proliferation and migration of periodontal ligament cells. Platelet rich growth factor can regulate the osteocalcin expression while adding to a culture with osteoblast-like cells. It is commercially available as GEM21s which is manufactured by molecular cloning process.39
2. Bone Morphogenetic Proteins (BMPs)
BMPs belong the superfamily of transforming growth factor-beta (TGF-β). In the human body BMPs are produced by the osteoblasts. BMP-2, -4, and -7 are naturally present in bone allografts and they can actively alters cell behaviour in vivo. Since the manufacturing of synthetic BMPs are a little bit expensive, their use in synthetic biomaterials are limited.40
3. Enamel Matrix Derivatives (EMDs)
Enamel matrix proteins are secreted by the Hertwig’s cells during the development of tooth. These proteins are then accumulated on to the root surface that influences the migration of the surrounding cells which promote the formation of cementum, periodontal ligament, and alveolar bone. Amelogenin, is a specific enamel matrix protein which assist in the mineralization of enamel. Amelogenin, under physiological conditions, assembled into nanospheres which during enzymatic degradation by metalloproteinases release bioactive peptides for weeks.41 This process stimulates new bone formation. Cambini et al.42 did a research regarding the application of amelogenin, its in situ persistence and their exceptional osteoinductive capability, which made the clinicians to avoid unnecessary use of barrier materials.
4. Demineralized Dentin Matrix
Demineralized Dentin Matrix scaffold, is produced from the patient’s own extracted teeth, is used to repair alveolar bone defects. Its structure and composition are similar to autogenous bone. It can be either in powder, block or moldable form and it can be mixed with hydroxyl propyl methyl cellulose for clinical applications in implant dentistry. Demineralised dentine matrix powder is prepared by crushing of dentin into smaller particles of 300–800 μm in size, and it contain dentinal tubule- approximately 50,000 tubules/ mm2. Animal studies of demineralised dentine matrix in a rat tooth which is milled to a size of 10–50 μm and mixed with hydroxypropyl cellulose as base material demonstrated bone formation, while hydroxypropyl cellulose, which is chemically stable in vivo, had an osteoconductive effect in the socket.43
Researches using transplantation of human dentin blocks (5–6 mm in diameter; 3 mm in thickness) for rabbit bone defects showed progressive dentin-bone ankylosis after 3 months, with osseous replacement and absence of inflammation. Furthermore, the use of porous dentin as scaffolds, support rapid microvascular ingrowth as well as osseointegration in mice highlighting their potential as bone engineering materials. Demineralised dentine matrix material exhibit osteoinductive, osteoconductive and act as a carrier for rh-BMP2.
The three dimensional (3D) printing technology enables the fabrication of scaffold with high precision there by allowing the creation of very detailed 3D structures. Inkjet printing, stereolithography, selective laser sintering and fused deposition modelling are some of the common techniques used to fabricate scaffolds. To achieve regeneration of complex tissue structures such as the periodontium, biomaterials are used as 3D templates for providing the extracellular matrix environment for the desired regenerative process.44
The main goal of implant dentistry is to delineate alveolar bone resorption and to establish masticatory function and aesthetics thereby maintaining the facial form of the patient. This can be achieved by gaining primary stability while implant installation. So quantity and quality of alveolar bone is one of the key stones for the success of the implants. The quantity of bone can be ascended by augmentation techniques along with various grafting materials.
Classical bone grafting materials used were having its own advantages and disadvantages. So recently advanced materials such as Demineralised Dentine Matrix proteins as scaffolds, incorporation of BMPs into graft materials, Enamel Matrix Derivative and Platelet Derived Growth Factor into alloplastic materials shows a tremendous revolution among properties of graft materials used in implant dentistry. Osteogenic properties of graft materials other than Autografts, can be improved by the recent innovations. Though the rate of resorption of graft materials and new bone formation are different with these materials, the incorporation of growth factors, stem cells and enamel and dentin enhances the alveolar ridge augmentation within time.
Augmentation procedures are inevitable in case of alveolar ridge resorption for implant treatment. So ridge preservation can reduce the horizontal and vertical bone alterations during implant therapy. There is no graft material developed until now which exhibit all the desirable properties simultaneously. Researches are running to obtain a material with superior properties so that clinicians can be guided to reach successful treatment plan and longevity of the implant prosthesis.