Dental lasers are becoming increasingly popular in dental practice since last few decades. They can be classified into soft tissue lasers and hard tissue lasers. Commonly used soft tissue lasers include Diode laser, Nd:YAG lasers and Carbon dioxide lasers since they are absorbed by the pigments in the soft tissues. Erbium family of lasers (Er:YAG and Er,Cr:YSGG) are good for ablating hard tissues such as tooth structure and bone since they are highly absorbed in water and hydroxyapatite. Comparing with other dental specialities, the use of lasers is not popular among prosthodontists due to lack of awareness. Prosthodontists also should accept laser technology as a proven method to treat patients safely and effectively with excellent results. Therefore, this article discusses the use and benefits of lasers in prosthodontics as well as the efficiency of this laser assisted procedures.
Laser is a new technology which is being used in clinical dentistry to overcome some of the drawbacks posed by the conventional dental procedures. The word laser is an acronym for the most significant feature of laser action: Light Amplification by Stimulated Emission of Radiation.1 The basic concepts of laser were first given by an American scientist, Charles Hard Townes in 1964. However, Theodore H. Maiman of California, was the first scientist who experimentally demonstrated laser by flashing light through a ruby crystal, in 1960.1
In this modern era, the success of prosthodontic treatment lies in restoration of function and esthetics to an optimum level. The patients demand optimal results with minimal effort. The proper use of lasers in prosthodontic practice can reduce number and length of appointment needed,accelerate healing and provide superior result.
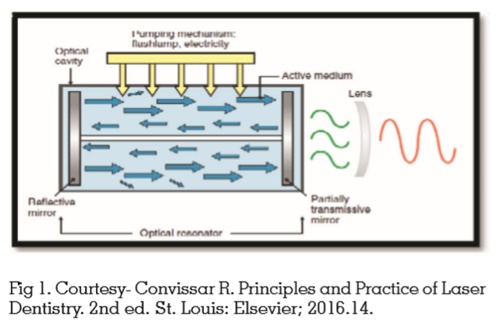
All laser devices have the following components (Fig 1)
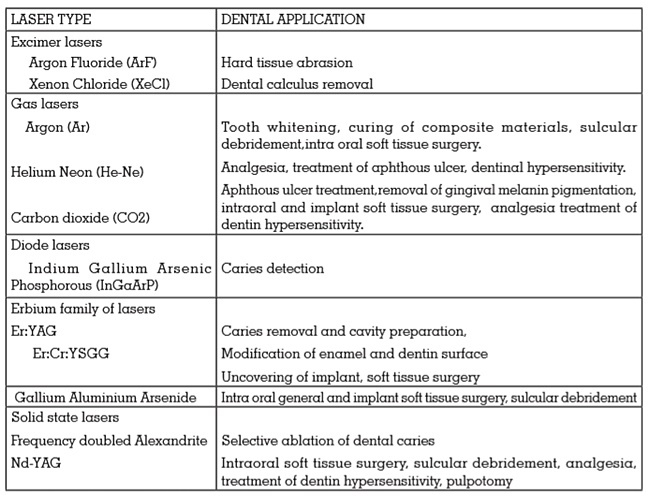
Mainly there are four types of laser delivery system which includes articulated arms, fibre optic delivery systems, hollow wave guide and water cooled fibreoptic system.3 Diode lasers and Nd:YAG lasers are available as fibre optic cables. CO2 lasers are delivered as hollow wave guide or articulated arm systems. Water cooled fibre optic delivery system is unique to the erbium family of lasers. CO2 and erbium lasers are absorbed by water which is a major component of glass fibers. Hence these lasers cannot pass through these fibers.5
Clinical advantages of dental lasers clearly benefit both patient and dentist. A clear field of vision resulting from moisture control and excellent hemostasis allows the dentist to perform all procedures with precision. Major advantages of dental laser include reduced intraoral bleeding, much less postoperative pain, and remarkably less post-operative swelling compared with conventional techniques such as electrosurgery. However, lasers have got some disadvantages. In some cases, the delivery system can be more cumbersome than an airotor or electric handpiece, and accessibility to the treatment area could be limited. The clinician must carefully monitor the rate of tissue removal to avoid overheating and lateral thermal damage. For enamel removal, the laser is not as fast as a conventional rotary bur, although it can be more conservative.
Lasers can be used as adjuncts to removable prosthetic care for many different procedures, including epulis fissuratum reduction, hyperplastic tissue reduction, vestibuloplasty, soft tissue/ osseous tuberosity reduction, torus/exostosis reduction, osseous adjustment of undercut and irregularly resorbed ridges, papillary hyperplasia, nicotinic stomatitis denture stomatitis and other pathologies under maxillary dentures.6
Soft tissue lesions
Hyperplastic fibrous tissue is formed at the junction of the soft and hard palate as a reaction to constant irritation and trauma from the posterior palatal seal area of the denture. The lesion may be removed with any of the soft tissue lasers and the tissue allowed to re-epithelialize.
The surgical correction of epulis fissuratum with suturing of the flap to the periosteum may fail because of excessive contracture of the vestibule with loss of vestibular height. This will result in a denture that does not properly fit in the vestibule. Lack of relapse,absence of scarring, good reepithelialization, and precise tissue destruction are the advantages of using a laser versus conventional techniques. Keng et al and Barak et al reported that the CO2 laser is ideal for this procedure.7
Vestibuloplasty
A common consequence of residual ridge resorptionis shallow vestibular depth, resulting in a inability to wear a denture with the desired function and comfort. Although this has been traditionally treated surgically, the CO2 laser is ideal in this situation for a bloodless vestibuloplasty, with excellent results.8
Tuberosity reduction
Soft tissue tuberosity reduction, when performed with laser is without any incision and suture. The soft tissue of the tuberosity is vaporized layer by layer until the correct interarch space has been achieved. Diode, CO2 or erbium lasers can be used. By using a laser, the treatment period was shortened by at least 3 to 6 weeks.9
Surgical treatment of tori, exostoses, undercuts and irregular alveolar ridges
Prosthetic problems may arise if maxillary tori or exostoses are large or irregular in shape or the mucosal covering becomes ulcerated. Hematoma formation is a common complication of surgical torus reduction. Whereas nohematoma formation during laser torus reduction has been reported. Combined use of erbium and CO2 helps in bony recontouring and hemostasis.10
The use of laser wavelength as an adjunct to restorative procedures can enhance the accuracy, predictability, and speed of treatment. The use of lasers in fixed prosthodontics include troughing / gingival retraction, hard and soft tissue crown lengthening and ovate pontic site preparation.11
Gingival tissue retraction:
On gingival tissue laser application was made possible by using flexible optical fibres (320-400microns) which ensures high precision of laser action at gingival sulcus level. Argon laser energy has peak absorption in haemoglobin, thus providing excellent haemostasis and efficient coagulation and vaporization of oral tissues. These characteristics are beneficial for retraction and haemostasis of the gingival tissue in preparation for an impression making during a crown and bridge procedure. It ensures “sterility” of the field, leading to superior gingival health around the margins.
Crown lengthening:
Lasers can be very efficaciously used for crown lengthening in situations of gingival overgrowth or passive eruption causing problem for tooth preparation during fixed partial denture procedures. Soft tissue procedures can be done with any of the soft tissue lasers. Osseous recontouring is done with erbium family of lasers. After surgery, provisionalize the area, and allow 3 to 4 weeks for healing before final impression.
Ovate pontic design:
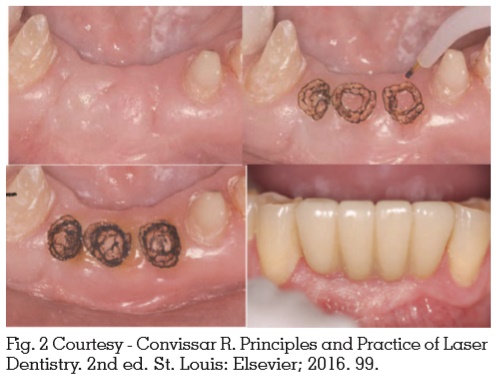
The ovate pontic site preparation using a laser starts with the removal of tissue from the center of the site. The diameter of the ovate site is slowly increased in a circular manner, ending it within 2mm from the adjacent mesial and distal abutment teeth. The interproximal papillae can be developed by leaving 2mm of gingival tissue mesially and distally. Various hard tissue and soft tissue lasers can be used for this (Fig 2).
Lasers can be remarkably useful in implant dentistry from surgical placement, to prosthetic delivery, to treating infected peri implant tissues. It include preparation of surgical site, decontamination and immediate implant placement, osteotomy, block graft procedures, lateral window sinus lift, second stage uncovering and photodynamic therapy in mucositis and periimplantitis.12 The advantages include increased hemostasis, minimum damage to the surrounding tissue, reduced swelling, reduced infection, and reduced pain postoperatively. Due to the hemostasis provided by the lasers, there is a significant advantage of improved visibility during surgery. The erbium family of lasers, with their hard tissue ablation action is used for osteotomy as well as decontamination of infected and ailing implant bodies.
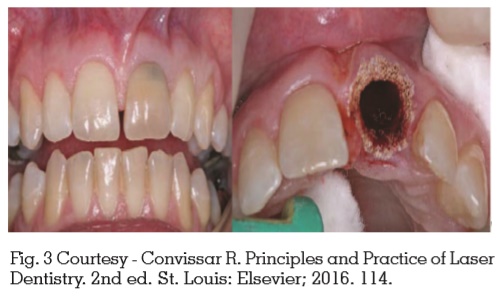
Preparation and decontamination of surgical site and immediate implant placement (Fig 3).
Lasers present a perfect solution to the problem of surgical site contamination. The soft tissue can be sterilized more effectively with laser before osteotomy than with rinsing or swabbing. Moreover, if saliva contaminates the surgical site during the procedure, it would be simple to release the area and re-establish sterility so that the procedure can be continued with the greatest chance for success.
Another situation requiring decontamination involves extracting teeth and placing implants immediately into the extraction site. In some cases, there might be the presence of infected tissues or soft tissue around the apices of roots or in the furcation area of molars. The erbium lasers are effective in removing the soft tissue remnants and decontaminating the bony surfaces at lower power settings with a water-coolant spray. Erbium wavelengths would leave the bone surfaces bleeding since they are not as effective as other wavelengths in creating hemostasis which is helpful in healing of the socket, when a graft or implant a is placed. The CO2 lasers are also a good choice because they will remove all soft tissue tags and decontaminate bony surfaces, again at low power densities. However, CO2 laser has excellent haemostatic property, so the effect of hemostasis on the tissues should overcome for healing.13
Osteotomy
In soft tissue “punch technique” if the tissue is thin (1-2 mm), any wavelength is acceptable. If it is thicker, using a diode or Nd:YAG laser may take minutes or seconds for erbium and CCO2O2 lasers. Depending on the quality of tissue, bleeding might be a problem with erbium lasers. The unobstructed vision, excellent hemostasis,and efficiency of cutting through all tissue thicknesses makes the COCO22 laser most suitable for these procedures.
Erbium family of lasers can be used to ablate bone. Laser ablation is less damaging to osseous tissues than surgical techniques, since it is a noncontact procedure without any friction between laser tip and bone. Friction from the bone cutting drills may overheat the bone and cause necrosis at the bone-implant interface. The temperature increases in osseous tissue while using an erbium laser is minimal if the clinician is familiar with the proper laser parameters and uses an adequate water spray. Thus, controlled ablation without any thermal damage of the tissue is achieved. Laser techniques has not advanced to the point where the entire osteotomy can be completed with erbium lasers.
Second stage uncovering of implants
This can be accomplished with any laser wavelength except Nd:YAG laser, because of its adverse effects on dental implants. If the soft tissue is not too thick (1-2 mm), all wavelengths except Nd:YAG can be used. If the tissue is significantly thicker, the diode laser would become too slow and inefficient. If the tissue is extremely vascular, the erbium laser is a poor choice because bleeding might obstruct vision. The CO2 laser is most efficient to remove thick soft tissue quickly and maintain unobstructed vision of the surgical site. Some implant designs might exhibit the large volumes of soft tissue. This tissue must be shaped to allow for impression making, abutment seating, and crown cementation.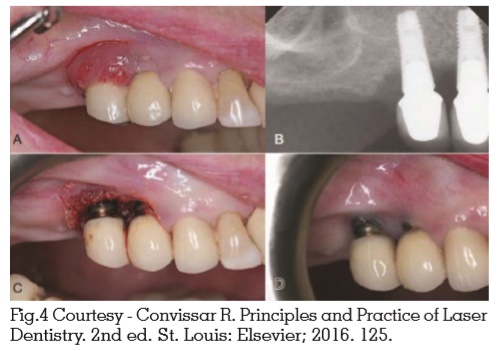
Mucositis and peri implantitis (Fig. 4)
Lasers provide a newer and better treatment modality for patients with mucositis and periimplantitis. Erbium laser, CO2 or diode laser can be used for this purpose. CO2 laser may be reflected off the surface of the implant and vaporize the bacteria in deep bony lesions, leading to a more thorough decontamination of the implant site. This leads to favourable conditions for healing and reosseointegration.
Photodynamic therapy
Photodynamic therapy is a technology based on the production of free oxygen radicals capable of affecting the membranes of microorganisms. The technique composed of a photosensitizer such as toluidine blue that can be activated by light of specific wavelength. The activated photosensitizer produces energy capable of transforming the surrounding oxygen into free radicals; the free radical then attacks the exposed microorganisms. Photodynamic chemotherapy may be used in dentistry to reduce the bacterial load in cases of immediate implant placement in infected socket and for the treatment of periimplantitis.14,15
Lasers in implant manufacture
Lasers have been used for deposition of hydroxyapatite (HA) films on titanium implants. Pulsed laser deposition (PLD) has proven to be a promising method to produce pure, adherent and crystalline HA coatings which show no dissolution in a simulated body fluid.16
Laser surface digitizing tools can be used to obtain to pologic data of the patient’s deformity, the procedure is called Laser Holography Imaging. Lasers help in creating a visually realistic prosthesis that shows an illusion of normal appearance. Laser technology has showed to be helpful for designing the position and shape of the prostheses. Lasers can avoid the need for conventional impression techniques and associated disadvantages like distortion of the soft tissue and irritation to patients. Lasers also overcome the disadvantages of 3D, CT and MRI reconstruction as the patient is not exposed to considerable radiation and any stress.17
The surface treatment of titanium castings to improve bonding with porcelain have shown improved bond strength when compared to conventional acid etching techniques. Lasers can also be used for welding, prototyping and computer aided design and computer aided manufacturing (CAD/CAM) technology, analysis of occlusion by CAD/CAM, analysis of accuracy of impression by the laser scanner, laser titanium sintering – direct metal laser sintering and laser welding of titanium components of the prostheses.18
The addition of laser treatment modalities to regular dental practice enhances a dentist’s ability to perform more clinical procedures with increased confidence and keep the procedures in office instead of referring to specialists. The increased patient awareness of laser treatments intensifies the patient-dentist relationship for comprehensive treatment.