Rehabilitation of congenital cleft palate defects improves the quality of life for the patient as normal as possible. The difficulties of cleft palate patients not only impairs the physical activities such as eating, breathing and speaking, but their psychological well-being is also affected. Thus, it has been recommended that a prosthesis may improve both the physical and psychological performances of patients, as well as their quality of life. In Velopharyngeal defect, hypernasality, regurgitation of food and liquids are the common consequences if left untreated. A maxillary hollow bulb obturator for these defects will prevent fluid leakage through nose, maintains cleanliness, speech resonance,improves physical and psychological health and mastication. This case report describes an edentulous cleft palate patient, which was rehabilitated with tooth supported maxillary hollow bulb obturator
Key words: Cleft Palate; Velopharyngeal defect; Metal coping; Hollow obturator.
Maxillary defects can be sourced by congenital malformations or the acquired defects resulting from surgeries, trauma etc. Patients with cleft palate may not been seen regularly in general dental practice, but is a frequent congenital anomaly affects 1 in 800 live births. The two prime objective of maxillofacial-prosthodontist for rehabilitation of the maxillary defects is to restore the functions of mastication, deglutition, and speech and to achieve normal oro-facial appearance.1 Defect of the maxilla, may be closed with an obturator, which is a disc or plate, natural or artificial. The obturator prosthesis that close these defects and separate the oral and nasal cavities may be constructed in different sizes and shapes, depending on the extent of the defect. Obturators are classified as solid, open hollow and closed hollow as to the nature of their extension into defect site. Both open and closed hollow obturators allow for the fabrication of a lightweight prosthesis that can be tolerated by the patient while effectively extending into the defect.2, 3 The retention of a complete dentures predominantly comes from the proper border seal and intimate fit of the denture base. Due to loss of teeth and posterior palatal insufficiency, the retention will be compromised. The present case report describes the rehabilitation of a patient with palatal insufficiency prosthodontically with a tooth supported closed hollow bulb obturator to improve the retention and function.
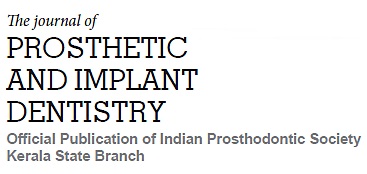
A 60 year old male patient reported to the department with the chief complaint of difficulty in chewing. General physical examination did not reveal any abnormalities and on oral examination there was partially edentulous arches with repaired cleft lip, nasal twang in his voice lacking resonance. Intraoral examination revealed a partially edentulous maxilla with Veau’s class III defect i.e. a defect of soft and hard palate extending floor of the nose. The remaining teeth present in both maxillary and mandibular arch were periodontally compromised with few sound teeth. Bony undercuts were observed in the tuberosity region. Considering the socio-economic condition, functional and esthetic requirements, tooth supported closed hollow bulb obturator was planned for the patient.
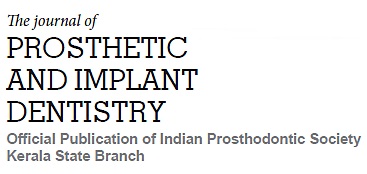
Prior to the treatment procedures, the mobile teeth and root stumps in the maxillary and mandibular arch were extracted resulting in a completely edentulous mandible and retention of 14, 15 and 23 in the maxilla (Figure 1a & b). For providing adequate support for the prosthesis rather than the tissue and bony undercut, the retained tooth in the maxilla were planned to be taken as a support. For that endodontic treatment was initiated for the remaining teeth and the tooth was prepared into a dome shaped to receive a metal coping. (Figure 2)
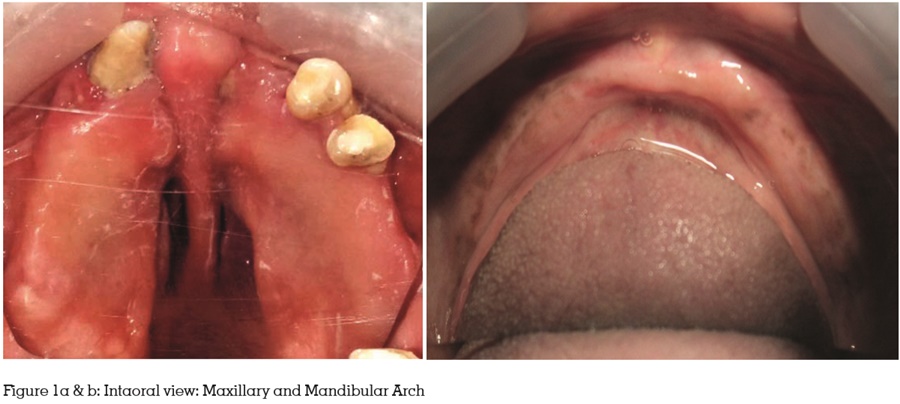
A gauze strip soaked was packed into the alveolar cleft area prior to impression making to prevent the impression material from being forced into the nasal cavity. A preliminary irreversible hydrocolloid impression (Algitex, DPI) was made in a stock perforated metal tray. The lower edentulous ridge was recorded with the same. The impressions were poured with dental stone to obtain primary casts.(Figure 3)
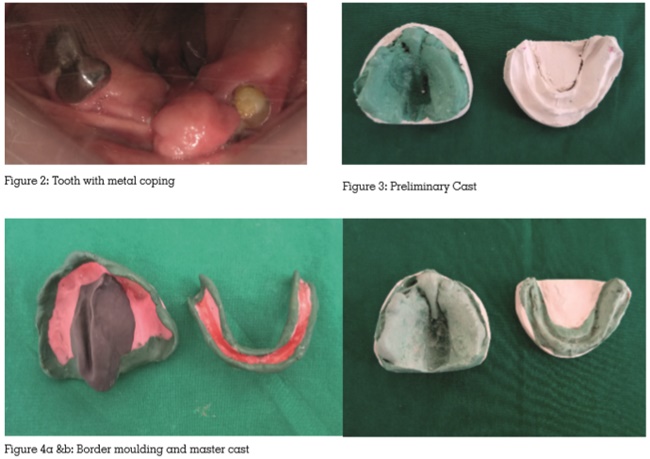
The blockout was done for the undesired undercuts and custom trays of auto polymerizing resin with a 2 mm wax spacer were fabricated over the primary casts. The tray extensions were then adjusted in the patient’s mouth and border molding was done using low-fusing compound (DPI Pinnacle tracing sticks). The defect portion was moulded using admix impression technique ( three parts of impression compound and seven parts of tracing compound) by extending head as far forward and backward as possible, making the patient move head in a circular manner from side to side and to say ‘ah’ and swallow. The border molding was continued until the contours of the defect were satisfactorily molded and a complete peripheral seal was obtained. The patient was able to speak, swallow and breathe through the nostrils effectively. Lower border molding was done following the routine technique. Final impressions were made with alginate in the maxillary arch and using Zinc-Oxide Eugenol in the mandibular arch. Master casts with dental stone were then obtained. (Figure 4a & b)
Following this, baseplate was adapted and wax occlusal rims were fabricated. Jaw relation records were made and artificial teeth arrangement was done. After try- in the master cast was duplicated inorder to obtain working cast. In the working cast the defective area was waxed up, cured and polished. (Figure 5a & b)
The finished bulb was adapted on to the master cast and the base plate with teeth arranged was placed and waxed-up. It was then flasked and dewaxed. To make an obturator portion hollow, lost salt technique was followed. In bulb portion, table salt was filled up to palatal plane and normal packing was performed with denture base acrylic resin. The lower complete denture was polymerized following the conventional technique. After that curing was performed, deflasking, trimming and polishing was carried out. After finishing and polishing, holes are placed in palate region and salt is removed with a syringe filled with water to make obturator in the bulb portion hollow. Following this, holes were filled with auto polymerizing resin (Self cure acrylic repair material, DPI). (Figure 6a –d)
The prosthesis was then inserted in the patients’ mouth and the extensions, speech, occlusion and esthetics were evaluated (Figure 7) Retention were improved with the incorporation of tooth with metal coping and from the tuberosity area. Necessary adjustments were done. Patient was happy as there was a considerable improvement in esthetics. Patient was followed up after 1 week and 2 weeks. Necessary denture corrections were done during the follow up visits.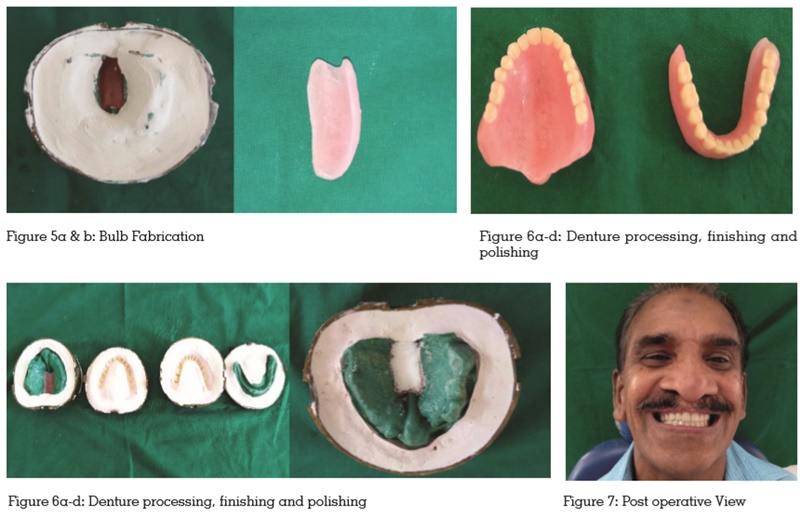
For alleviating any functional or anatomical defects in the oral structures, definitive prosthodontic treatment is one of the practical approach that can be advocated when surgery is not considered as an option. Traditionally, the congenital palatal anomalies are best treated with open or closed hollow obturators. Hollow bulb provides advantages such as reduction in weight, increased retention, and makes prosthesis comfortable. Closed hollow bulb obturators has added advantage of preventing fluid and food accumulation, reducing airway space, and allow for maximum extension.4, 5
The prosthodontist plays a significant role in the rehabilitation of palatal defects. Rehabilitation of an edentulous patient with congenital maxillary defect with an obturator is arduous as the patient have to face difficulties from the initial stages of impression making till the denture insertion. The basic design of the obturator prosthesis made use of the available tissue bearing area and extending into the defect to engage the undercuts to achieve maximum retention and stability. Along with the bony and tissue undercuts, the presence of few teeth in the above mentioned case enhanced the retention even more making it into a tooth supported definitive closed hollow bulb obturator. Taking into consideration the different domains of care, definitive prosthesis gives the patient an opportunity to live life as near normal as possible with good function and esthetics.6