Osseodensification is a recently introduced interesting technique that enhances the bone density around dental implants and increases the primary stability. It is well established that implant stability is critical for osseointegration. It is directly related to surrounding bone quantity and quality. Maintaining and preserving bone during osteotomy leads to increased primary stability, mechanical properties and bone to implant contact, thereby enhancing secondary stability and healing.
Osseointegration is a prerequisite for successful
implant treatment. The term Osseointegration was
coined by Brånemark (1985).1 Primary stability
of dental implants has been considered as an
important factor for achievement of successful
osseointegration and thereby secondary stability.2
Primary stability has a direct relationship
with density of bone. Thus maintenance and
preservation of bone or the compaction of less
dense bone during osteotomy facilitates enhanced
primary stability and Bone to Implant Contact
(BIC). The main concept of osseodensification
technique is that instead of bone excavation, the
drill design allows densification of the osteotomy
site walls by compaction and autografting of bone
tissues in an outwardly expanded direction.3
Dental implant stability is the measure of the
anchorage quality of an implant in the alveolar
bone. Implant stability can occur at two different
stages: primary and secondary. It has been proven
to affect the process of osseointegration, the pattern
of implant loading, and, finally, the success of an
implant.
Primary stability of an implant mostly comes from
mechanical engagement with cortical bone. Thus it
prevents the formation of a connective tissue layer
between implant and bone, ultimately ensuring
bone healing.4 Secondary stability, on the other
hand, offers biological stability through bone
regeneration and remodeling.[4 HYPERLINK “http://www.
jdionline.org/article.asp?issn=0974-6781;year=2012;volume=2;issue=2;spage=1
03;epage=109;aulast=Rao”]
Degree of implant stability may also depend
on the condition of the surrounding tissues. The
quantification of implant stability at various time
points helps to predict the long-term prognosis.1
A secure primary stability leads to a predictable
secondary stability.
The key factors in enhancing implant primary
stability are bone density, surgical protocol, implant
thread type and geometry. Poor bone density is
associated with excessive bone resorption and
will impair bone healing, therefore considered as a risk factor for implant failure.
The posterior maxilla has a thinner cortical bone
and thicker trabecular bone when compared with
mandible, which has thick cortical bone. Hence the
chance of implant failure in posterior maxilla is
more. So it is always desirable to have a technique
to improve the density of osteotomy site.
Implants of parallel, cylindrical and tapered
designs are available in market. Parallel design
implants are not appropriate for most applications.
Tapered designs provide a degree of compression
of the cortical bone in an implant site with
inadequate bone.
Implant surface topography and roughness also
have an effect on the healing process by promoting
favorable cellular responses and cell surface
interactions. Rough implant surface will allow
a firm mechanical contact with the surrounding
tissues due to its larger surface area. Sandblasted
implant surfaces enhance the growth and metabolic
activity of osteoblasts by promoting peri-implant
osteogenesis.
Primary stability can be improved by increasing the bone to implant contact by various methods
such as adapting to surgical techniques and by
implant selection.
The use of thinner drills and wider and tapered
implant designs will result in lateral compression of
the bone trabeculae, an increase of the interfacial
bone stiffness and primary stability.5 Under
preparation of the implant bed is another widely
used surgical technique to improve the implant
stability. This is usually achieved by using one
or more sizes smaller last drill than the implant
diameter.6 Surface texturing of implants may
reduce the risk of stability loss thereby facilitating
osseointegration. Certain studies also show that
bicortical anchorage improves the primary stability
of apical portion of implants.6
Traditionally, standard osteotomy drills are used
to excavate bone from the implant osteotomy site.
But the imprecise cutting of the osteotomy drills
makes the design elliptical or elongated, which
will reduce the torque during implant placement.
This ultimately contributes to poor implant stability.
Osteotomies tend to fracture the bony trabeculae,
resulting in long remodeling time and delayed secondary implant stability.
Also, osteotomies prepared in deficient bone or
narrow ridges may produce buccal or lingual
dehiscence that necessitates additional bone
graft increasing the healing period and cost.
Some cases might require sinus lift procedures,
which require a separate appointment. Because
of these limitations, a newer biomechanical bone
preparation method called “osseodensification”
was introduced into the field of implant dentistry.
Dr. Salah Huwais developed osseodensification
in 2013 using specially designed burs (Densah™
burs) that help densify bone as they prepare an
osteotomy. It is a bone non-excavation technique.
The procedure is characterized by low plastic
deformation of bone that is created by rolling
and sliding contact using a densifying bur that is
fluted such that it densifies the bone with minimal
heat elevation.7
Due to osteoblasts nucleating around the bone
which is in close proximity with the implants,
osseodensification will initiate new bone growth
formation. It will densify the bone contacting the
implant. There is a need for ≥2 mm of trabecular
bone core and more than 1:1 trabecular/ cortical
bone ratio to achieve a predictable plastic
expansion. This technique is indicated in narrow
crest with wider base. It facilitates lateral ridge
expansion if the ridge width ≤3 mm. It is used for
maxillary sinus autografting where it facilitates
vertical ridge expansion. It is not indicated for
resorbed ridge with narrow base.
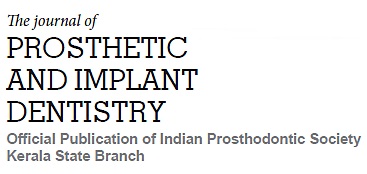
Densah burs (Fig 1) are special burs having the
ability to expand narrow bone ridges similar to
split crest techniques. They increase bone density
in the peri-implant area & thereby improving the
implant mechanical stability of dental implants.
Osseodensification does not excavate the bone but simultaneously compacts and autografts the
particulate bone in an outward direction to create
the osteotomy, thereby preserving vital bone tissue.
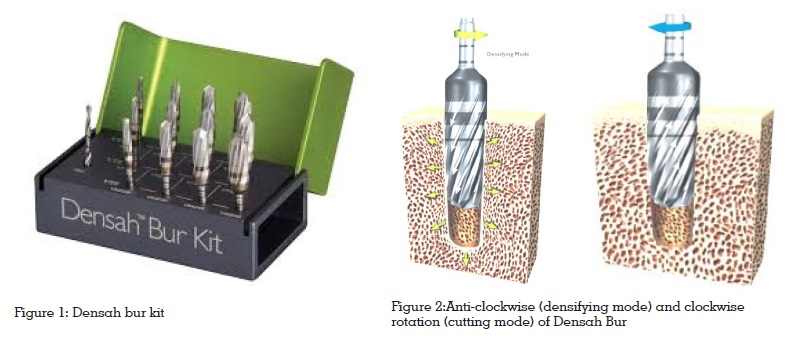
These burs rotate both in clockwise (cutting mode)
and counterclockwise (densifying mode) direction
simultaneously at a speed of 800-1500 rpm with
steady irrigation (Fig 2). In clockwise direction,
it will cut the bone precisely along the created
osteotomy walls and in anti-clockwise direction, it
will densify the precisely cut bone. Thus, the bony
fragments will act as an autograft maintaining
the bulk of bone.
This pumping motion (in and out movement)
creates a rate-dependent stress to produce a
rate-dependent strain and allows saline solution
pumping to gently pressurize the bone walls.
This combination facilitates an increased bone
plasticity and bone expansion.6 This will increase
the residual strain. Huwais demonstrated that
osseodensification helped ridge expansion while
maintaining alveolar ridge integrity, thereby
allowing implant placement in autogenous
bone, also achieving adequate primary stability.
Osseodensification helps in preserving bone bulk
and shortened the waiting period to restorative
phase.8
This technique cannot be used in cortical bone, as
the cortical bone is a non-dynamic tissue, which
lacks plasticity. Xenografts should not be used
for densification as they behave biomechanically
different than the bone tissue. They contain only
inorganic content that provide the bulk without
any viscoelasticity.2
Placement of dental implants in poor density
bone (D3 and D4 bone type) is always arduous
in implantology as it compromises primary
stability of dental implants. Osseodensification,
a bone non-excavating technique can be used
in low bone density ridges. It not only improve
primary stability and bone contact through the reversed compression exerted due to elastic bone
spring back effect but also densify the bone due
to instrumentation related autografting.9 The
Densah burs by rotating in both clockwise and
counterclockwise direction will precisely cut and
densify the bone, thereby increasing the bone
bulk. This ultimately increases the primary stability
of dental implants placed in low density bony
ridges. Therefore, it is time to think about bone
preservation to enhance its ability to heal faster,
regardless of implant macro- or micro-geometry.8