Cranioplasty is a surgical intervention utilizing
an implant material to repair cranial defects
both functionally and aesthetically. The cranial
implant not only protects the brain but also provide
cosmetic results. The most important advantage
of cranioplasty is it improves the neurological
deficit by decreasing local intracranial pressure
besides improving the dynamics of CSF changes1.
Cranioplasty can also aid in postural blood
regulation, cerebrovascular reserve capacity
and glucose metabolism within the brain. This
article presents the rehabilitation of a patient with
acquired skull defect using custom made titanium
implant prosthesis.
A 32 year old male patient reported to the
Department of Prosthodontics, Government Dental
College, Kottayam referred from the Department
of Neurosurgery Government Medical College,
Kottayam for the management of an acquired
cranial defect. The patient had a previous history
of road traffic accident (RTA), resulting in an open
head injury with right temporo-parietal contusion
and fracture of the squamous part of temporal
bone. The patient was treated immediately with
a right fronto-temporo parietal craniotomy by the
neurosurgeons. Post operatively it was found that
the patient had lateral hemiplegia on the left side and a large bony defect of 15cm × 12 cm size on
the right side of the skull [Fig-1]. It was planned
to close the defect using custom made titanium
cranial prosthesis.
The construction of any maxillofacial prosthesis
with an alloplastic material consists of several
stages, each of which is equally important to the
success of rehabilitation. These stages include
moulage impression, working cast fabrication,
sculpturing the pattern, mould fabrication and
processing of the final prosthesis2. Impression
procedure was planned at the first scheduled
appointment. Patient was instructed to report
after shaving off hair from the face and head
to facilitate impression procedure. Accuracy of
delineating margins of the cranial defect is an
important step in impression procedure. This was
achieved by palpating the margins of the defect
and marking 2-3 mm beyond the outermost borders
of the cranial defect using an indelible pencil.
Once the margin of the defect was established,
modeling wax (MAARC-MODELLING WAX) was
adapted along the periphery to limit the flow of
irreversible hydrocolloid impression material.
(DPI- NEW ALGITEX) [Fig-2]. Petrolatum jelly was
painted on the tissue further for ease of removal
of impression material. A thin mix of (DPI- NEW ALGITEX) impression material was then carefully
poured onto the defect area taking care to avoid
air trap [Fig. 3]. After placing cotton tufts onto
the setting impression material, a second pour of
lightly mixed plaster of Paris was placed over it to
provide support to the impression material [Fig. 4].
Once the impression material was set, it was
removed carefully, evaluated and poured with
type 3 dental stone (GOLD STONE-GREEN STONE
PLASTER) to obtain the master cast. Outline of the
defect marked on the tissue which was transferred
on the impression was highlighted with indelible
pencil, so that this marking could be transferred
to master cast, for fabrication of wax pattern [Fig. 5]. The master cast was painted with separating
medium for ease of removal of wax pattern.
The design of the final cranial prosthesis was
discussed with the neurosurgeons, and the wax
pattern was fabricated following the contours of the
skull on the master cast. On the second scheduled
appointment wax pattern was tried on to evaluate
the fit along the margins of the defect. The contour
of the wax pattern was corrected from all the three
sides(frontal, sagittal and occipital) to restore
the normal contour and appearance [Fig. 6]. A
titanium cranial prosthesis was fabricated from
the wax pattern [Fig. 7]. The patient was again
recalled for trial of the custom made titanium cranial prosthesis to check for shape and fit of the
prosthesis from all the anatomical aspects [Figs.
8, 9].
The surgical procedure involved the preparation
of scalp with an antiseptic solution and the
reflection of the scalp with a U shaped incision
to completely expose the bony margins of the
defect, titanium screws were used to secure the
titanium prosthesis into the exact position and
the defect was closed [Figs. 10, 11, 12]. A closed
system suction drain was placed immediately after
surgery to reduce the postoperative hematoma.
The drain was removed after 48 hours following
which the patient had a good recovery. The patient and his parents were instructed for the care of the
reconstructed area. Post surgically the contour of
the defect was satisfactorily reconstructed from
all the anatomical aspects.
Besides protection of the underlying brain, the
prosthesis helped to repair the contour of the
vaults providing satisfactory esthetics [Figs. 13].
Cranioplasties have been performed since the
early 1950s1. Many different types of materials
were used throughout the history of cranioplasty.
The advancement in biomedical technology, have provided new materials for prosthetic rehabilitation
An ideal cranioplasty material must have the
following features5.
More importantly, a cranioplasty material that
fulfills all these characteristics is yet to arrive.
Common materials used in the field of cranioplasty
are4, autografts (cranium, tibia, rib, scapula, fascia,
sternum, ilium), allograft, xenograft, nonmetal
allograft (celluloids, methyl-methacrylate, hydroxyl
apatite, polyethelene,silicon, choral, cortoss,
ceramic), metal allograft (aluminium, gold, silver,
tantalum, stainless steel, titanium, lead, platinum,
vitallium, ticonium) and polyether ether ketone
(PEEK) etc.
Developments in endoscopic equipment have
given the surgeons the opportunity of minimally
invasive cranioplasty technique called endoscopic
cranioplasty. With endoscopic tools materials
such as acrylic and hydroxyapatite can be
administered through small incisions. Although
minimal invasiveness is an advantage, there is
still lack of evidence from large patient group to
support this method.
Interests in acrylic resins among neurosurgeons
increased considerably following Spence’s 1954 report of a simple method for fabricating implants at
the time of surgery, using auto polymerizing methyl
methacrylate3. Advantages of acrylic implants are
dimensional stability, non-conductivity, lower cost
and ease of modification and placement4. However
methyl methacrylate can cause exothermic
reactions, which may damage the surrounding
tissue and lead to subgaleal exudative fluid and
infection6,7. The major advantages of titanium over
methyl methacrylate are low modulus of elasticity,
low density and very low rate of corrosion. Besides
this it is nontoxic, elicits no inflammatory reactions
and has an infection rate under 2%7,8,9. Moreover, it
is robust enough to resist secondary trauma while
providing maximal stability of the cranial vault5.
Holes of 2mm dimensions were drilled onto the
surface of the titanium prosthesis to prevent the
development of epidural hematoma and allow for
ingrowth of fibrous connective tissue to assist in
stabilization. Furthermore, the holes help to secure
the prosthesis to the bony defect10.
Although computer aided design and
manufacturing (CAD-CAM) generated titanium
cranial prosthesis have been introduced, the cost
of this prosthesis is a major concern.
Researches on both biologic and non-biologic
substitutes for cranioplasty are going on worldwide.
Stem cell experiments and development of
morphogenic proteins are expected to take place
in the short-term future4.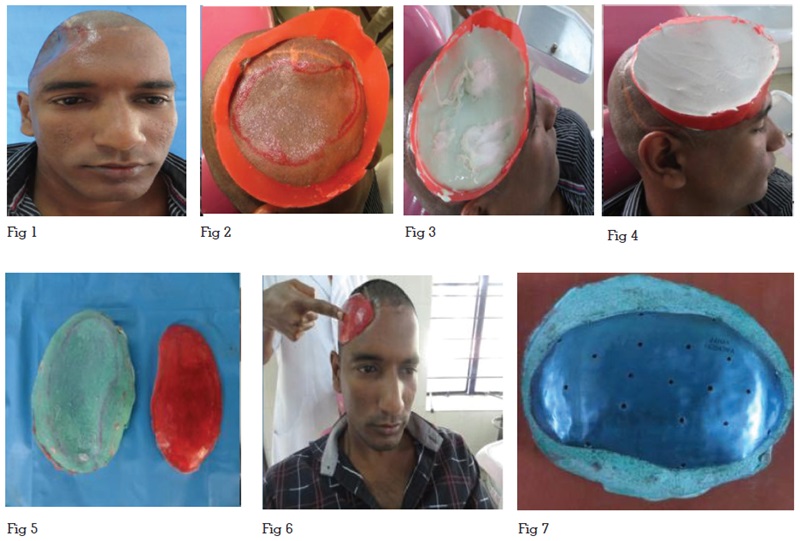

Cranioplasty is one of the most common surgeries
performed in trauma settings. Rehabilitation of
cranial defects using custom made titanium cranial
prosthesis will reduce adjustment of prosthesis
during the surgery. This case report describes an
effective, economical and simple technique for
rehabilitation of a person with acquired skull defect
using a custom made titanium cranial prosthesis.