ABSTRACT: Dentures can produce various changes in the oral environment which remains unforeseen in most of the cases. As denture is the main reason behind denture stomatitis, proper oral and denture hygiene should be maintained in order to avoid this condition. In the present review article various etiological factors, physiology, clinical features and treatment modalities of denture stomatitis are discussed.
Key words: Denturestomatitis, poor oral hygiene, candidialinfection, chronic atrophic candidiasis, inflammatory papillary hyperplasia.
Denture stomatitis indicates an inflammatory
process of the mucosa that bears a complete or
partial removable dental appliance, typically a
denture. Incidence of occurrence is 11-67% in
complete denture wearers. Denture stomatitis
is also known by the names Denture sore
mouth, inflammatory papillary hyperplasia,
denture induced stomatitis and chronic atrophic
candidiasis. Success in the treatment of complete denture patients requires not only mechanical
skills and proficiency but also a knowledge of the
physiology of the involved anatomical structures
and an understanding of the possible pathologic
changes that may occur after the treatment.
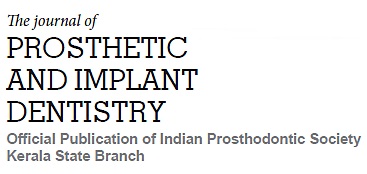
Clinically Denture stomatitis appears in various types. Some authors have classified Denture stomatitis into:
The causative factor for Denture stomatitis is multifactorial. Some authors believe that there is no primary etiological factor behind it. Other factors thought to be particularly significant is:
1. Candidial infection:
Cahn (1936) 1st proposed
that infection by candida albicans were responsible
for denture stomatitis. Factors responsible for
colonisation of candida species in fitting denture
surface are adherence of yeast cells, Interaction
with oralcommensal bacteria, Redox potential of
the site, Surface property of acrylic resin. Factors
that increase the susceptibility to candida –
associated denture stomatitis includes aging,
malnutrition , immunosuppression, radiotherapy,
diabetes mellitus, and treatment with antibacterial
antibiotics.
According to Boucher’s 12th edition factors
predisposing to denture stomatitis are:
Systemic-old age, diabetes mellitus, nutritional
deficiencies (iron, folate, vitamin b12
deficiency), malignancies (acute leukaemia,
agranulocytosis), immune defects, corticosteroids,
immunosuppressive drugs.
Local-Dentures(changes in the environmental
condition, trauma, denture usage, denture
cleanliness), xerostomia (sjogren’s syndrome,
irradiation, drug therapy), High carbohydrate diet,
Broad spectrum antibiotics, Smoking tobacco.
2. Denture trauma (including continuous denture
wearing): According to Nyquist:
Dental trauma
plays a prominent role in the aetiology of denture
stomatitis. It plays vital role in Type 1 & least
important in other types of denture stomatitis2,3. Some researchers believe that the lesion occurs
less frequently under ‘non-traumatic dentures4.
Also it is less frequently seen in patients with
satisfactory alveolar ridges compared with those
with flat ridges4,5. Continuous wearing of denture
might cause denture stomatitis6.
Incorrect vertical dimension of occlusion has also
been suggested as a contributing factor. The result
of the studies by Emami E et al.., research suggest
traumatic occlusion results in an inflammatory
reaction which may create an environment
favourable for microorganisms found in denture
stomatitis.
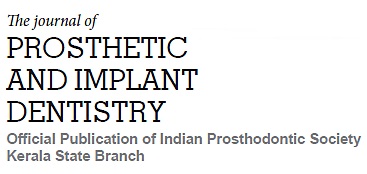
3. Denture cleanliness(including reaction to denture
plaque):
Poor oral hygiene is the most frequently
involved local aetiological factor in denture
stomatitis4,7. Denture provide opportunities for
food lodgement and prevent the natural cleansing
action by tongue, lips & cheek8,9. Poor oral hygiene
is the major factor in candida related lesions.
Denture cleaning methods may affect the condition
of dentures, and pigmentation and abrasions in
dentures occur with the use of toothpaste or hard
tooth brush10: (Walker, British dental journal,1981).
Poor oral hygiene, high carbohydrate intake,
reduced salivary flow, composition of saliva, design
of prosthesis, continuous denture wearing enhance
pathogenicity of dental plaque. (fig.4)
4. Allergic and primary irritant reactions to denture
base materials:
Toxicity is usually manifested by
the release of several chemical constituents from
the material, which can induce an allergic response
in terms of localized or generalised stomatitis.
This reaction may be related to presence of resin
monomer, hydroquinone peroxide, dimethyl-ptoluidine
or methacrylate in denture. Contact
sensitivities are more common to occur with cold
or auto polymerized resins than with heat cured
denture base materials.
5. Systemic factors
including predisposing factors.
Changes in the oral physiology of
importance
Wearing of dentures imposes a marked change
in the environmental conditions of the denture
supporting tissues. Inconvenience caused by the
initial insertion of denture, by excessive salivation
is a transitory condition and compensation occurs
within two weeks. Asialorrhea makes the denture
retention difficult and predisposes to oral mucosal
irritation. Due to the microbial degradation of
carbohydrates contained in saliva film and in the
material adherent to denture base material, there
is lowering of pH of saliva in between denture base
and supporting tissues, which is a predisposing
factor for Monilial infections. If the denture bearing
tissues are nutritionally deficient, the prosthesis
will fail even if how well it is constructed.
Denture bearing area
Thin and friable epithelium covering the edentulous
saddle area may not be able to tolerate the forces
imposed upon it by hard unyielding acrylic. Also
the connective tissue pad in between the bone and
the epithelium covering may not be thick enough
to absorb the forces placed upon the area.
Oral environment
Oral environment must be moist and warm and
the oral mucosa must be firm elastic and able
to resist mild abrasions, to keep the prosthesis
comfortable. If the mouth is dry and the tissue
burning and friable, it is almost impossible for the
patient to tolerate even if the denture is perfectly
balanced and carefully constructed.
Dehydration
As elderly people are susceptible to negative
water balance, especially due to excessive water
loss through insufficient or damaged kidneys, the
oral mucosa also becomes dry-easily dehydrated.
Saliva
Xerostomia results when water is reduced, resulting
in reduced water content in saliva, which in turn
affects the mastication.
Dry mouth
Mucous membrane becomes hot, dry and fragile
in dry mouth, which cannot be tolerated by denture
wearers. Even most skilfully fabricated denture
fails in dry mouth cases.
Osteoporosis
Osteoporosis results from the loss of bone especially
the spongy spicules of bone that support the weight
bearing parts of the skeleton. Osteoporosis is
common in ageing person, especially in postmenopausal
women when the osteogenic blood
level has dropped precipitously.
Thinning of mucosa
The epithelium becomes very thin in elderly; hence
a prosthesis placed upon the edentulous ridge is
now covered by a thin pad of connective tissue
rests mostly on bone. It is uncomfortable the hard
acrylic or metal base rest almost directly upon
the bony ridge with little cushion effect between.
Therefore the search for soft acrylic base to cushion
the occlusal force continues.
Female predilection is seen in case of denture
stomatitis. The Mean age is approximately 49
years (mean age at which a person start to wear
denture).Common Site is under complete or partial
denture, mainly in palatal areas. Appears as
patchy distribution often associated with speckled
curd like white lesion.
28-70% of patients with denture stomatitis have
oral complaints11,12: (Nater; J Pros Dent, 1978). The
symptoms include mucosal bleeding, swelling,
burning or painful sensation, halitosis or an unpleasant taste & dryness in the mouth. Signs
that are clinically present include bright red,
oedematous and granular palatal tissue, Red
patches which appears erythematous or speckled,
sharply outlined border of reddened mucosa which
are restricted to the tissue in contact with the
denture and multiple pinpoint foci of hyperaemia
are seen.
Clinically an erythematous area under the complete
denture aid in diagnosis of denture stomatitis.
Confirmed by- mycelia or pseudo hyphae in a
direct smear or high number of candida species
from lesion (>50 colonies)
Yeast recovered from the fitting surface of the
denture confirms, candida is the main cause of
denture stomatitis.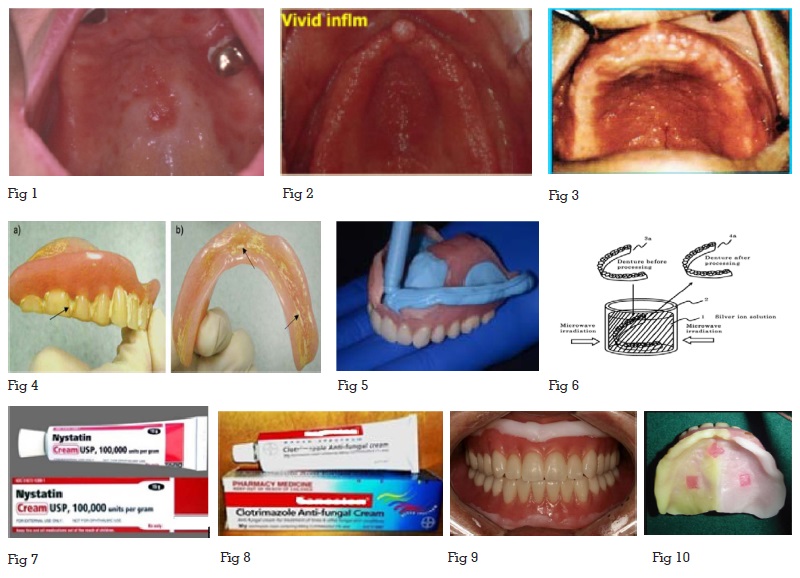
In this context, incorporation of antifungal agents
into the denture base materials to be progressively
released into the oral cavity has been suggested
to prevent the biofilm accumulation, inhibit
C.albicans colonization and contribute to the
treatment of Denture stomatitis. This protocol
requires only the use of denture by the patients,
thus reducing the need for patient compliance to
antifungal drug regimes.
Furthermore, the incorporation of drugs into
denture liners breaks the contact between the
denture biofilm & infected tissues, thus avoiding
a cycle of re-infection via prosthesis, hence soft
lining materials are highly recommended. In order
to avoid degradation & microbial colonization antimicrobial
agents are added to lining materials,
mainly short term ones as tissue conditioners
& temporary resilient liners which are more
susceptible.
Although anti-fungal/anti-microbial effectively
inhibit the growth of Candida albicans, it may
affect their morphological structure, hardness, roughness, properties such as tensile strength, water
absorpotion, modulus of elasticity and weight, and
peel bond strength to denture base resin. Hence,
Bueno, et al. determined minimum inhibitory
concentrations (MICs) of C.albicans biofilm for
antifungal/antimicrobial agents added to the
lining materials. Five drugs-nystatin, miconazole,
ketoconazole, itraconazole and chlorhexidine
diacetate are the drugs usually incorporated.
During their life cycle, polymeric materials release
soluble substances like methyl methacrylate &
dibutyl phthalate, which may be potentially toxic.
So; it is possible to conclude that modification
of temporary resilient materials by antifungal/
antimicrobial agents, especially in lower
concentrations, may represent a viable protocol
for treatment of denture stomatitis during a period
similar to conventional therapy with topical
antifungals (14 days). (fig.10)
Denture placement in the oral cavity will produce
notable variations in the oral microbial flora
affecting the integrity of oral tissues. Hence
adequate home care instructions should be given
at the time of denture delivery. Regular recall
appointments to reinforce denture hygiene.
In most cases elimination of traumatic factors,
adequate oral hygiene measures, administration
of local antimycotic medicaments enables the
healing of denture stomatitis.