According to WHO1, 17.9 million people die each year from cardiovascular diseases(CVDs), an estimated 31% of all deaths worldwide. It is estimated that approximately 46.9% of the patients are affected by CVD in India.2
Evidence suggests that eventhoughpeople are living longer, it is accompanied by different health problems3. Edentulismis a common condition which has considerable impact on quality of life of an individual4,5. Dental implants are fast becoming the best novel method to confront edentulism. The possibility that the impaired blood supply and the consequent hypoxia may negatively affect the healing process of bone around implants may cause a higher risk of implant failures in patients with cardiovascular diseases6.
The different forms of CVDs like hypertension, atherosclerosis, vascular stenosis, coronary artery disease and congestive heart failure can havedirect effect on blood tissue supply through different mechanisms7. Wound infection is prevented by the presence of adequate oxygen which increases fibroblast activity, collagen synthesis, capillary growth, and macrophage activity8,9. Hypoxia can lead to a decline in the fibroblast activity, collagen synthesis, capillary growth, and macrophage actions10, which in turn is expected to influence the osseointegration of dental implants.
In contrast to these problems in CVDs, there is scarce information about thefailure of dental implants in patients with CVDs.A systematic literature search of MEDLINE and EMBASE database from 1985 to 2019 was performed. All searches were performed using medical subject heading (MeSH) or free text words (Box 1).This article provides an overview of the literature to update the knowledge to decideif dental implants are contraindicated in CVDs.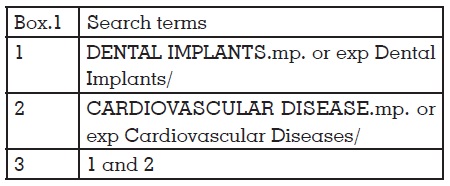
A major challenge when it comes to addressing the CVDs is the vast majority of diseases in it. Hwang and Wang10,11 have given a list of medical conditions which are considered absolute and relative contraindications for dental implants. According to which the CVDs which are absolutely contraindicated include recent myocardial infarction or a cerebrovascular accident, vascular prosthesis and bleeding associated with any of these problems.
Myocardial infarction (MI) (ie, heart attack) is the irreversible death (necrosis) of heart muscle secondary to prolonged lack of oxygen supply (ischemia)12. If a patient has had a recent myocardial infarction, it can generate necrosis and functional deficits due to prolonged ischemia. It is found that about 75% of such patients experience complications within a short period after the incident13.
Cerebrovascular accident (CVA) is the medical term for a stroke. A stroke is when blood flow to a part of your brain is stopped either by a blockage or the rupture of a blood vessel14. It is found that death occurs in 15% of the patients within the first 3 months. The functional recovery in such patients varies from the first month to a year ahead. This time period is crucial as it is prone to numerous dangerous complications15.
In these two conditions, patient stability occurs with intervention and a healing period of 6-12 months after preliminary care. The interim period of 3-6 months after primary stabilisation, is of prime importance as there is a chance for complications. Thus, any procedure which induces stress must be avoided in this time period. Any procedure to be done should be done only after 6 months with medical consent11.
Another important factor is the medications taken by such patients. A clinician must always be aware of the anticoagulant or thrombolytic therapy administered to the patient. Evaluation of INR is necessary to prevent complications due to the intake of such medications11.
Bioprosthetic valves are used in heart valve replacement. They generally offer functional properties (eg, hemodynamics, resistance to thrombosis) that are more similar to those of native valves. Treatment of hemodynamically significant aortic or mitral valve disease by implantation of prosthetic has become increasingly common16. The three forms of prosthetic valve include bioprostheses, mechanical valves, and homografts or autografts. Among which all except autografts are more prone to cause endocarditis, as well as regurgitation, stenosis, and degeneration.
It is seen that the prevalence of endocarditis is maximum during the first 3 months after the placement and it reduces by 6 months17. This is attributed to the healing of the tissues around the valve which encloses the valve, thus protecting against microbial action18.
A patient who had a prosthetic valve replacement stabilises only after 6 months of the procedure17,18. Any procedure which can cause bacteremia must be avoided during this time period. Alongside, based on the type of the valve (mechanical or bioprosthesis [porcine]), used, the patients are advised different drug regimens (anticoagulants or plasma volume elevators, respectively)18 in accordance to it. A clinician should be aware of such medications and the precautions to be taken before any invasive procedure in such patients.
Bleeding: It is important to ensure there is proper hemostasis before any elective surgery is done. Hemorrhage is attributed to a multitude of factors like platelet disorders or clotting factor disorders. But the most common reason for bleeding is the use of drugs which can cause the same. Intake of anti-coagulant drugs necessitates the monitoring of bleeding time as well as INR value. It is proposed that a patient with INR value of 3 or less can undergo procedures like dental extraction, by use of transexamic acid or epsilon aminocaproic acid to control residual bleeding from the site19. If a patient is advised to keep the INR value above 3, dental implant placement is not advisable.
Another important factor which is to be considered is the platelet count. Decreased platelet count can lead to bleeding during the procedure or postoperatively. It depends upon the platelet count in the patient. Etiology of decreased platelet count includes infection, idiopathic thrombocytopenia purpura, radiation therapy, myelosuppression, and leukemia11. Mild thrombocytopenia can cause abnormal postoperative bleeding; whereas a platelet count below 50,000/mm3 can lead to major post-surgical bleeding and a count below 20,000/ mm3 can cause spontaneous bleeding of the mucous membrane. These patients usually require perfusion if surgery is to be done20.
Hematocrit is the volume percentage (vol%) of red blood cells in the blood. It is important as any patient who has to undergo sedation or general anesthesia necessitate at least 75 to 80% of the normal value of haematocrit. Thus, hematocrit becomes important when the level is below 60% of the normal value21.
CVDs such as dysrhythmia or heart murmur does not have a significant effect on the healing process. This is due to the fact that in some of these diseases, blood pressure does not change, and in others, heart function is normal22. Therefore, these diseases, might not have an effect on the osseointegration of dental implants.
In spite of all the physiologic variations happening due to CVDs, they are found to have no effect on the success of dental implants. A retrospective cohort study by Moy et al in 200523 evaluated the risk factors for dental implants. The results show that among the 1365 implants placed in patients with coronary artery disease or hypertension, the implant failure was similar to control patients, thus showing there is no contraindication in placing dental implants in such patients.
Alsaadi et al24 in 2007 has shown that there is no risk of early implant failures associated with hypertension and coagulation problems which was followed by another study25 in 2008 which has shown no association of hypertension and coagulation problems with late implant loss.
In contrast to these studies, a retrospective study26 has shown a higher risk of implant failure in CVD, in consideration with the number of implants placed, with no association with increased periimplant pathology, but Krennmair et al27 found that there is increased risk of bone loss in CVD. Later, Pedro et al28 and Niedermaier et al29 found that the survival rate of implants in CVD was not different from normal patients, thus dental implants are not contraindicated in CVDs.
There is very scarce evidence which shows Cardiovascular diseases to be an absolute contraindication. The literature suggests that dental implants can be placed in patients with CVDs provided proper precautions are taken in conditions which are detrimental. A few precautions include,