In this modern era, newer technologies and their applications improve the predictability and outcome of the conventional procedures to a great extent. Lasers are introduced into the field of dentistry in 1989, which is widely used in all branches of dentistry. In this article, the scope of lasers in various aspects of prosthodontics is discussed.
Currently, various laser systems are available for use in dentistry. Neodymium-doped: Yittrium- Aluminium-Garnet (Nd: YAG), carbon dioxide (CO2), semiconductor diode lasers,Erbium doped: Yttrium-Aluminium-Garnet (Er:YAG) and Erbium doped: Yttrium –Scandium-Gallium- Garnet (Er:YSGG) have already been approved by FDA. The introduction of lasers into the field of prosthodontics has replaced many ordinary surgical and technical methods and has improved the quality of treatment rendered to a patient. Stability, retention, function and esthetics may be enhanced by proper laser integration in both the soft tissue and hard tissue procedures.
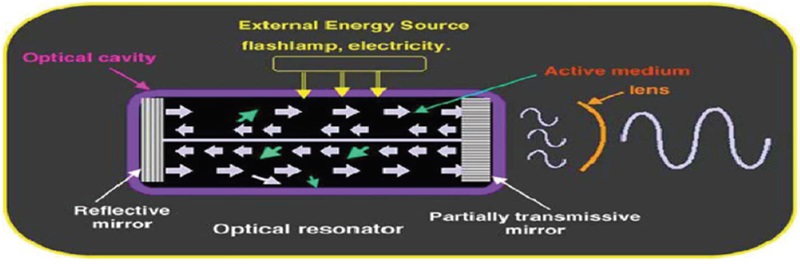
Laser is the acronym for “Light Amplification by Stimulated Emission of Radiation” named by GORDON GOULD in 1957. A study of each words offers an understanding of the basic principles of how a laser operates.
Light is a form of electromagnetic energy that behaves as a particle and a wave. The basic unit of energy is called a photon2. Laser light has one specific color, a property called monochromacity. Laser light possesses three additional characteristics: collimation, coherency, and efficiency.
A quantum which is the smallest unit of energy, is absorbed by the electrons of an atom or molecule, causing a brief excitation; then a quantum is released, and the process is called as “spontaneous emission”. Albert Einstein summarised in his theory that an additional quantum of energy traveling in the field of the excited atom that has the same excitation energy level would result in a release of two quanta, a phenomenon called stimulated emission2. This process will occur just before the atom can undergo spontaneous emission.
The photons are then reflected back and forth within the active medium to further enhance stimulated emission, and successively passes through the active medium and ultimately collimate the photo beam2. This is the process of amplification.
Radiation refers to the light waves that are being produced by the laser as a specific form of electromagnetic energy2. The electromagnetic spectrum is the entire collection of wave energy ranging from gamma rays, whose wavelength is about 10-12 nm, to radio waves, whose wavelength can be thousands of meters. All the available dental laser devices have emission wavelengths of approximately 0.5 μm (or 500 nm) to 10.6 μm (or 10,600 nm)
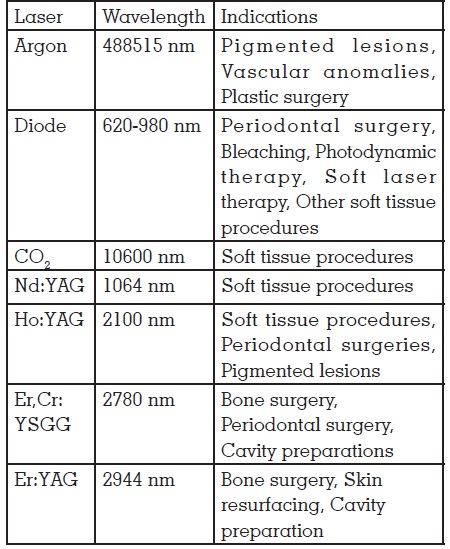
Traditionally, laser have been classified according to the physical construction of the laser (e.g. gas, liquid and solid state), the type of medium which sustain lasing3. Several types of dental lasers are available based on the wavelengths:
The lasers used in dentistry are illustrated as follows:
Lip and gingival hyper pigmentation is an issue in young adults when the dark brown pigmentation gives an unsighty appearance. Diode lasers can be used for depigmentation of dark coloured gingiva and lip4. Pink esthetics has to be established before going for restorative procedures.
The laser is selectively absorbed by the melanin that causes pigmentation. This leads to a photothermal ablation of melanocytes which leads to its disruption and subsequent removal by the body’s immune system4. Lasers produce a blood less field for surgery,minimal heating of surrounding tissue, causes minimum damage to periosteum and underling bone and mucosa do not need any dressing. It destroys cells at the basal layer thus reduces repigmentation.
When some patients have an uneven gingival line producing an uneven smile, excessive tissue can be easily and quickly removed using diode lasers without the need for blade incision. This creates a blood less field which allows for immediate impression making. Here steps for hemostasis is not needed. There will not be much recession of gingiva and repositioning of soft tissues. This also eliminates the problems associated with conventional surgery or electrocautery3,5,6
This is a procedure done when inadequate crown height is present for crown restoration. An adequate crown height is created by removing either gingival soft tissue or bone or both. The diode or CO2 lasers can be used for soft tissue removal and Argon lasers for hard tissue removal or both can be done using Erbium lasers. The thermal effect of laser seals vascular and lymphatic vessels and at the same time vaporize the excess gingival tissue. Since no flap was raised, sutures were not necessary and the wound healed by secondary intention. For Erbium lasers coagulation tendency is less compared to CO2 and diode lasers. So hemostasis procedures are necessary before impression making3,5,6.
Frenectomy using lasers can be done for the following situations
The argon laser is a valuable tool in performing frenectomy procedures. While the argon laser is very effective in cutting fibrous tissue at higher energies, it is also particularly beneficial for lingual frenectomies, because of the haemostatic properties. The use of argon laser during these procedures results in efficient tissue removal with a bloodless field. Excellent haemostasis occurs, sutures are not required, and the patient experiences minimal discomfort during the healing period6
Harmonisation of pink and white esthetics has become important in modern society. Bleaching with diode lasers results in immediate shade change and less tooth sensitivity and is preferred among in office bleaching systems. All the bleaching procedures should be carried out before restorative procedures3,5.
Erbium lasers can be used for tooth preparation for laminates which will produce an etched tooth surface. The finish line has to be refined using carbide burs
Lasers like Er:YAG and ErCr:YSGG can be used to remove unwanted or failed veneers due to cement discolouration or tooth discolouration. Restoration can be removed with the help of laser beams without any cutting. The laser energy passes through the porcelain glass unchanged and is occupied by the water molecules present in the adhesive. Debonding takes place at the silaneresin junction without causing any trauma to the underlying tooth1,7
Continuous and persistent trauma from a sharp denture flange or over compression of the post dam area may produce a fibrous tissue response. Hyperplastic fibrous tissue may be formed at the junction of the hard and soft palate as a reaction to constant trauma and irritation from the post dam area of the denture. The lesion may be excised with any of the soft tissue lasers and the tissue allowed re-epithelialized. Lesions like epulisfissuratum, denture stomatitis can also be corrected using lasers.6,11
Application of lasers on gingival tissue was made possible particularly by the use of flexible optical fibers (320-400 microns for prosthetic applications) ensuring high precision of laser action at crevicular sulcus level3. Sulcus conditioning with laser is an innovative method in the process of restoration with a fixed prosthesis, and the ever increasing operator interest in its atraumatic properties has made its development possible. It is also known as laser troughing11.
Argon lasers have peak absorption of hemoglobin, thus lending itself to provide excellent hemostasis and efficient coagulation and vaporization of oral tissues. These characteristics are beneficial for retraction and hemostasis of the gingival tissue in preparation for impression making during a crown and bridge procedure (Kutsch, 1993).
Laser-based techniques have been in use for many years with extremely predictable results. The advantage of laser prosthetic/cosmetic reconstruction surgery over traditional techniques is documented strongly in the literature12. The addition of laser treatment modalities will enhance the dentist’s ability to perform more clinical procedures, increase confidence and experience, and keep the procedures in office instead of referral to specialists. In general, increased awareness of laser treatments as reported in today’s media has intensified the contribution of the patient, within the patient–dentist relationship, in determining comprehensive treatment.