Biocompatibility is a property of implant material to show favourable response in given biological environment. In order to replace a missing tooth, many biomaterials have been evolved as implants over many years in an effort to create an optimal interaction between the body and the implanted material. With all the advances and developments in the science and technology, the materials available for dental implants have also improved. Selecting the appropriate implant biomaterial is a key factor for long term success of implants.
A dental implant is a prosthetic device made of alloplastic material implanted into the oral tissues beneath the mucosal or periosteal layer and or within the bone to provide retention and support. Historically it was postured as a therapy of last resort, after all other options of treatment had been exhausted. Today American Dental Association and many dental educators view dental implants as devices that can be used in selected cases with great care taken to properly inform the patients about the benefits and risks involved. In this context it is imperative to know about the biomaterials, their history, properties, types, biocompatibility and future of dental implant.
2500 BC - Ancient Egyptians - wedged a number of materials into sockets like shells, wood and carved ivory1,3
500 BC - Etruscan population – used gold bands along with pontics
500 BC - Phoenician population used gold wire.
300 BC - Phoenician population - Carved Ivory teeth.
600 AD - Mayan population - implantation of pieces of shell.
1700 - John Hunter – transplantation of the teeth1,3,4.
1809 - Maggiolo - pieces of gold.
1911 - Greenfield - iridoplatinum basket is soldered with 24 carat gold.
1939 - Strock - vitallium screw to provide anchorage for replacement.
1940 - Formiggini - spiral implant - stainless steel wire1,3,4
1943 - Dahl -Subperiosteal type of implant.
1948 - Goldberg- Extension of frame work.
1952 - Branemark- Threaded implant design1,3
Early 1960s - Chercheve –double helical Spiral implant made using Cobalt Chromium.
Early 1970s - Grenoble –implants made of vitreous Carbon
1970 and 1980 - Weiss and Judy - Titanium Mushroom shaped projection
Late 1970s and Early 1980s - Tatum - custom blade implants of Titanium alloy
Early 1980s - Tatum - Titanium root form implant
After 1980s –Hollow basket Core vent implant, Screw vent implant, Screw vent implant with Hydroxyapatite coating, Implant with titanium plasma spray
Dental Implant Materials
Metals and Alloys- Titanium & Titanium –6 Aluminum-4Vanadium (Ti-6AI-4V) and Commercially Pure Titanium, Cobalt-Chromium- Molybdenum-Based Alloy, Iron-Chromium-Nickel- Based Alloys
Ceramics-Aluminium, Titanium and Zirconium oxide, Bioactive and biodegradable ceramics
Carbon --Carbon & carbon silicon, Vitreous and Pyrolytic
Polymers and Composites- Polymethylmethacrylate (P M M A) , Polyethylene ( U H M W- P E ) , Polytetrafluoroethylene (PTFE), Silicone rubber, Polysulfone)1
Bone Augmentation Materials
Ceramics -Calcium phosphate, Bioactive glass & glass ceramics
Polymers -PMMA, Lactic/glycolic acid
Natural Minerals -Collagen, Demineralizedbone matrix, Bone morphogenic proteins1
Classification of implant bomaterials2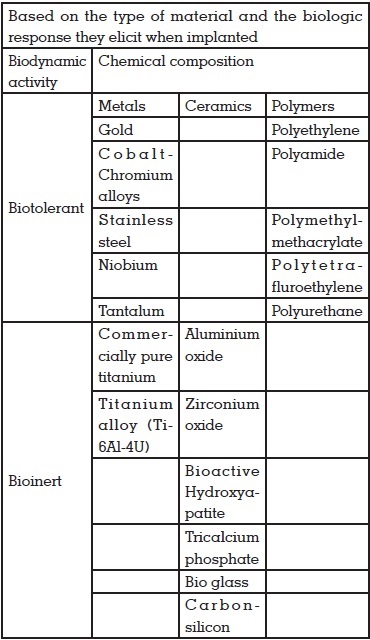
Materials used for the fabrication od
dental implants5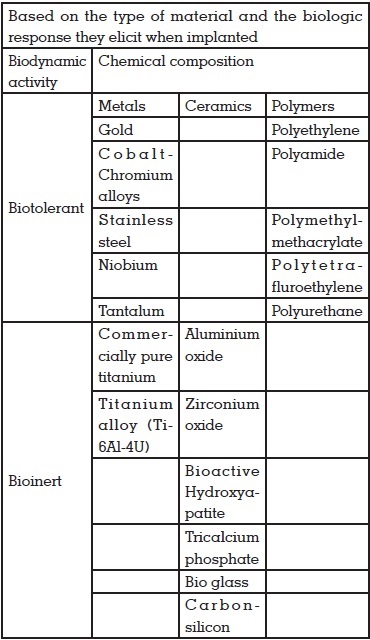
Mechanical properties
i. Modulus of elasticity: Should be equivalent to bone (18 GPa). It is selected for equal stress distribution at implant and to reduce the mobility of the implant
ii. Tensile, shear, and compressive strength: Should essentially be high to prevent implant failure
iii. Yield and fatigue strength: Should be high to prevent brittleness of the material
iv. Ductility: Minimum of 8% is required as per American Dental Association (ADA) for coining of the implant.
Chemical properties
Corrosion is defined as loss of metallic ions from the surface of a metal to the surrounding environment. There are four types, namely, pitting corrosion, crevicecorrosion, galvanic corrosion, and electrochemical corrosion.
i. Pitting corrosion: It is a rapid process which occurs in an implant with small surface pit which when placed in a solution, the metal ions which are present near to the pit dissolve, thereby losing its positive ions and combines with chlorine ions leading to pitting corrosion
ii. Crevice corrosion: It occurs at the bone–implant interface. When metallic ions dissolve, they create positively charged environment, thus resulting in crevice corrosion
iii. Galvanic corrosion: The difference in electrical gradients results in galvanic corrosion. The ions which get leaked into saliva at the implant interface later pass on to peri‑implant tissues, thus leading to implant failure as a result
iv. Electrochemical corrosion: With the presence of passive oxide layer at the implant metal surface,anodic oxidation and cathodic reduction can be prevented to a greater extent.
Metals and alloys
On the long run, the conventional metals (gold, stainless steel,and cobalt-chromium) have become outdated and are now replaced by titanium (Ti) and its alloys (mainly Ti-6Al-4V)1,6.
Titanium alloys are light, strong and highly resistant to fatigue and corrosion, six times stronger than compact bone and offer more opportunities for designs with thinner sections. When compared with Co-Cr-Mo alloys, titanium alloys are twice as strong and have half the elastic modulus. And also titanium shows a relatively low modulus of elasticity and tensile strength when compared with most other alloys6
Ceramics
Aluminium oxide (Al2O3)
Zirconium oxide
Hydroxyapatite (HA)
Tricalcium phosphate
Tetracalcium phosphate
Calcium pyrophosphate
Fluorapatite
Brushite
Bioglass etc.
Ceramics are inert to biodegradation and possess high strength and other physical characteristics suitable for implant application. Aluminium, titanium, and zirconium oxide have a clear, white cream or light grey colour that is beneficial for application on anterior root form devices. They have minimum thermal and electric conductivity, biodegradation, and reaction to bone, soft tissue, and oral environment are also considered to be beneficial when compared with other types of synthetic biomaterials6,7
Materials made of Calcium phosphate (CaPO4) such as tricalcium phosphate (TCP) and glass ceramics have excellent biocompatibility, no local or systemic toxicity, minimal thermal and electrical conductivity, no alteration to natural mineralization process of bone, and lower mechanical,tensile, and shear and fatigue strength. Apart from the use as a bone substitute, calcium phosphates have been considered as a good option for implant coatings that may promote accelerated bone healing around implants6.
The latest ceramic to be used as dental implant is zirconia (zirconium dioxide). It is found to possess good mechanical properties owing to its multiphase structure. The metastable tetragonal phase stabilized zirconia will displaya stressinduced transformation toughening mechanism. The strength and toughness of zirconia can be accounted for by its toughening mechanisms such as crack deflection, zone shielding, contact shielding, and crack bridging. Preventing the crack propagation is of critical importance in high-fatigue situations such as mastication and parafunction. This combination of favourable mechanical properties makes zirconia a unique and stable material for use in high-load situations6,7.
Zirconia is radiopaque and clearly visible on radiographs. It’s ivory colour, is similar to the colour of natural teeth and is especially critical in the aesthetic zone with high lip line smiles. Zirconia is also proposed to accumulate lesser plaque than titanium. Furthermore, with the development of dental computer-aided design (CAD) computer-aided manufacturing (CAM) systems, this high strength ceramic is gradually becoming a satisfactory implant biomaterial7.
Polymers and composites
Polymeric implants in the form of polymethyl methacrylate (PMMA) and poly tetra fluoro ethylene (PTFE) were first used in the 1930s. Other types of polymers, which were used subsequently as dental implant material included polyamide, polyethylene (PE), polyurethane (PU),polypropylene (PP), polydimethyl siloxane, polysulfone (PS), and silicone rubber. In general, the polymers have lower strengths and elastic moduli and higher elongation to fracture compared with other classes of biomaterials. Most polymers have shown elastic modulus with magnitudes closer to soft tissues1,6,7
Titanium alloys (Ti–Zr and Ti–20Nb–10Zr–5Ta)
Ti–6Al–4V alloy is considered to be an alternative to cpTi because of it’s good mechanical and corrosion resistance and a much lower elasticity modulus. There have been attempts to further improve its properties like elastic modulus, corrosion resistance, and biocompatibility. There are reports that vanadium and aluminium ions can lead to neurological problems such as Alzheimer’s disease and adverse reactions in tissues over an extended period. So, the need for the development of new Titanium alloys, mainly with the addition of niobium, molybdenum, tantalum, and zirconium, i.e; elements that have no cytotoxicity. Alloys like Zr–Ti, Ti–Zr–Nb–Ta (TZNT) exhibits better physical, mechanical and biological properties than cpTi to be used as dental implant materials8,9.
Zirconia toughened alumina (ZTA) and alumina
toughened zirconia (AZT)
Another class of for dental implants is Alumina– Zirconia composites. They can be either Zirconia toughened Alumina (ZTA) when Alumina is the main component (70–95%), or Alumina Toughened Zirconia (ATZ), when Zirconia is the main component. The mechanical and tribological properties and biological safety of different ZTA and ATZ composites have been reported in many studies. The advantages are the combination of the characteristics of Alumina (high hardness, high stiffness) with the properties of Zirconia(high strength and high toughness, with improvement of slow crack growth resistance). Several studies on Alumina–Zirconia composites have shown the positive effect of Alumina on the hydrothermal stability of tetragonal Zirconia phase8,9
Zirconium alloy
Zr-based bulk metallic glasses (BMGs) is evolving as biomedical implants. Recently, a new Zr-based BMG, Zr61Ti2Cu25Al12 (ZT1), is developed. For most crystalline metals, reduction of the modulus is usually accompanied by a sacrifice in strength. Young’s modulus of the ZT1 BMG is about 20% lower than that of Ti and its alloys, more close to that of the bone, along with a large elastic strain limit. Biocompatibility of ZT1 was assessed by in vitro cytotoxicity testing. Cellular responses for three cell phenotypes, L929, HUVEC, and MG63, the phenomenological behavior of cells such as attachment, adhesion, spreading, and proliferation for the (ZT1) metallic glass is substantially comparable to the CpTi and Ti–6Al– 4V. Also,osteoblast gene expression of integrin b, alkaline phosphate, and type I collagen, mRNA level for the cells grown on ZT1 substrates is much higher than those on the CpTi and Ti–6Al–4V alloy8,9
Poly-ether-ether-ketone (PEEK)
Poly-ether-ether-ketone (PEEK) has been introduced to replace metallic implant components in orthopedics, traumatology, and for calvarial reconstructions. In dentistry, clips on implant bars and healing abutments are sometimes manufactured recurring to PEEK9,10.
PEEK is a semi-crystalline thermoplastic polymer, which has very good strength and stiffness along with an outstanding thermal and chemical resistance-e.g., against oils and acids. Being colorless and possess an elastic modulus close to that of the bone, PEEK is a viable option for dental implant manufacturing. PEEK alone is generally bioinert and is not conductive to cell adhesion. Recent studies have shown new processing and surface modifications that affect the biological and mechanical properties of pure PEEK9,12.
Bone augmentation materials
In 1923, Hegedus attempted to use bone grafts for reconstruction of osseous defects. This method was later brought back by Nabers and O’Leary in 1965.
Autologous or autogenous bone grafting involves utilizing the bone obtained from the same individual receiving the graft. Sources include iliac crest, mandibular symphysis (chin area), anterior mandibular ramus (coronoid process), and bone removed during osteoplasty and osteectomy11,12
Allograft is derived from humans itself. The difference is that bone is harvested from an individual other than the one receiving the graft. Allograft is taken from cadavers that have donated their bone11.
Xenografts are obtained from species other than human-like calf bone have been used to treat osseous defects. Currently bovine-derived bone Bio-oss has been used widely in periodontal defects and in implant surgery11
Hydroxyapatite (HA) composite is a synthetic variant which has a mineral to organic matrix ratio, approximating that of human bone. Artificial bone can be created from ceramics such as calcium phosphates (e.g., HA and tricalcium phosphate), bioglass, and calcium sulfate and is biologically active depending on the solubility in physiological environment11.
Growth factors-enhanced grafts are produced with the help of recombinant DNA technology. They consist of either human growth factors or morphogens like BMPs in conjunction with a carrier medium, such as collagen. These factors, residing in extracellular matrix of bone, include transforming growth factor-beta (TGF-β), insulinlike growth factors I and II, platelet-derived growth factor (PDGF), fibroblast growth factor, and BMPs11.
Platelet-rich fibrin (PRF) is a healing biomaterial with a great potential for bone and soft tissue regeneration without any inflammatory reactions, and may be used alone or in combination with bone grafts, promoting hemostasis, bone growth, and maturation12.
Implant is gaining much popularity and is becoming the first treatment option. The success behind dental implants is in selecting the right implant biomaterial. Both titanium-based alloys and zirconium-based ceramics possesses unique set of pros and cons. Zirconia-based ceramics have higher biocompatibility and better aesthetics as compared to titanium-based alloys. Titaniumbased implants represent significantly better mechanical properties, particularly fracture strength as well as a longer history of application and therefore, established reliability over time. The quest for a perfect biomaterial still continues.