Several studies have shown an association between ABO
blood types and susceptibility to certain infections. Other
investigators, however, reported that blood type O, or non
secretion of antigen might be a risk factor for increased
candidal colonization. As, not much of the literature is
available on such a relationship, this invivo study was
carried out to determine the relationship between degree
of denture plaque accumulation as one of the risk factor
for increased candidal carriage and ABO blood types
among denture wearers.
Aim: Was to determine the correlation between degree
of denture plaque accumulation and ABO blood types
in denture wearers.
Materials and method: Complete denture wearing patients
(n=210) with age range of 50-65 years reporting to the
department of Prosthodontics fulfilling the inclusion criteria
were included. Before start of the prosthodontic treatment,
demographic details as well as a questionnaire on the
concerned diseases and denture hygiene were recorded.
Denture hygiene was assessed by modified plaque index
(Tarbet) and blood groups were determined by direct
agglutination method.
Statistical analysis used: chi square, student t-test, one
way ANOVA and tukey HSD.
Result: Significant differences were observed in the degree
of denture plaque accumulation among various blood
groups.
Conclusion: Blood group O shows higher degree of denture
plaque accumulation (grade 3,4) as compared to other
blood groups. Research should be pursued in various
aspects of ageing and age related oral health problems,
including epidemiological studies to measure the burden
of oral diseases.
Key words: Candidiasis, colony forming unit (CFU), Denture stomatitis.
Candidiasis is a complex, multi factorial
process5,6,7,8 that occurs when the host defence
system is compromised. Presence of dentures
also serve as a predisposing factor for Candida
associated denture stomatitis.4 Both the plaque
accumulation on the denture and poor denture
hygiene contributes to the virulence of Candida
offering its clinical picture.4
Nikawa et al (1991) demonstrated inter relationship
between ABO blood types of denture wearers,
denture plaque accumulation and degree of oral
Candidal colonization.9 In Indian context, data
was lacking on such an association. So, study
aimed at looking into such association.
It has been reported that both the plaque
accumulation on the denture and poor denture
hygiene contributes to Candida associated denture
stomatitis and an inter relationship exists between
ABO blood types of denture wearers, denture
plaque accumulation and degree of oral Candidal
colonization. However, this relationship in clinical
dentistry has not been extensively studied. So, aim of this study is to determine the relationship
between degree of denture plaque accumulation
and ABO blood types among denture wearers.
This in vivo study “To determine the correlation
between degree of denture plaque accumulation
and ABO blood types in denture wearers” was
carried out in the Department of Prosthodontics
of the institute. It included 210 patients for
identification of denture hygiene and blood
samples using standard protocol by using- Direct
Heamagglutination test.
Materials used for collection of blood sample:
Blood grouping and typing reagent (Eryscreen,
India), Disposable gloves for Specimen handling,
Sterile disposable syringe with needle (two ml,
Dispovan, India), Glass slide (25x75 mm), Test
tubes (8x50 mm), Disposable applicator sticks,
Normal saline, Pasteur pipettes, Sodium or calcium
hypochlorite solution (five %) to wipe and disinfect
the spills, Disposable waste bag to collect and
dispose used accessories and waste
Source of data collection: Complete denture
patients (sample size of 210 subjects) reporting
to the department of Prosthodontics of the institute.
Inclusion Criteria: Subjects who give their consent
for the study. Completely edentulous, healthy
individuals with no denture wearing historycomprises
the control group (group A). Completely
edentulous, healthy individuals, with atleast six
months denture wearing history comprises the
study group (group B)
Exclusion Criteria: Subjects with any antifungal
therapy. Subjects with any systemic diseases
(immunocompromised, diabetics) or those
taking antibiotics for more than two weeks or
hypoglycaemic or hypertensive drugs. An informed
consent was obtained from these subjects before
carrying out the study.
COLLECTION OF SAMPLE: All complete denture
wearing patients reporting to the department
of Prosthodontics fulfilling the inclusion criteria
were included in the study. Before start of the
Prosthodontic treatment, demographic details as
well as a questionnaire on the concerned diseases
and denture hygiene was recorded. Before starting
the study, ethical clearance was obtained from
the institute. For assessing denture hygiene,
modified plaque index was used as described
by Tarbet. Blood groups were determined by direct
Heamagglutination method, using monoclonal
antibodies against human A and B blood group
antigens. (Department of Oral Pathology). Clinical
Assessment- Inspection of the condition of oral
mucosa was carried out under dental chair light.
Upper and lower complete denture evaluation was
done for grading their cleanliness according to
prosthesis hygiene index by Tarbet. In this method,
the maxillary denture was removed from the mouth
and soaked in a bowl of water for one minute to
remove food debris. 0.1% neutral red solution
was painted on the fitting surface and left for one
minute. The denture was rinsed under running tap
water to remove the unbound dye. The disclosed
denture plaque on the fitting surface of the denture
was then scored.
It is graded as:
• no plaque
• light plaque (25% of the fitting surface covered)
• moderate plaque (26- 50% of the fitting surface
covered)
• heavy plaque (51-75% of the fitting surface
covered)
• very heavy plaque (76-100% of the fitting surface
covered)
Observation and Result- This prospective study
was carried out to evaluate the relationship
between ‘ABO’ blood types and degree of denture plaque accumulation in denture wearers.
For the study, individuals requiring complete
dentures were selected at random from the O.P.D
of the department of Prosthodontics. Age range of
samples vary between 40 -90 years Sex predilection
favoured predominantly males.
Individuals requiring complete dentures with
at least six months of denture wearing history
comprise the study group (n=105). While, the
individuals with no denture wearing history
comprise the control group (n=105). Blood type
of each individual was then determined (Dept. of
Oral and maxillofacial pathology). The samples were again subdivided according to their blood
types (A/B/AB/O).
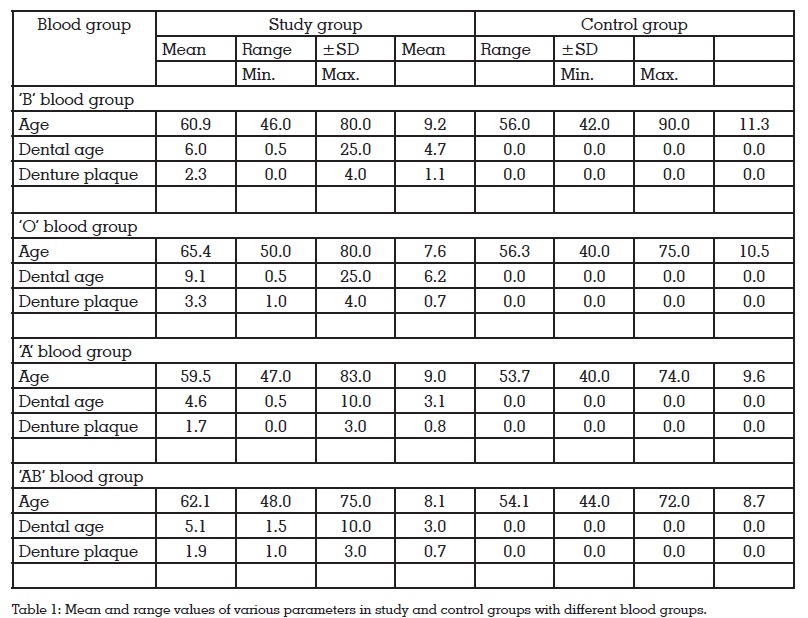
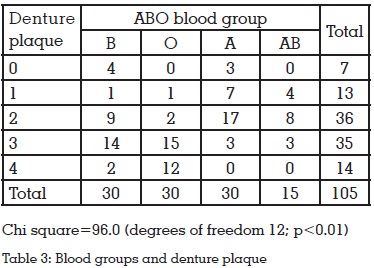
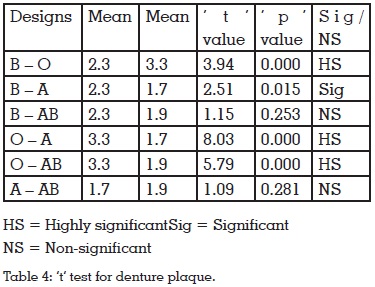
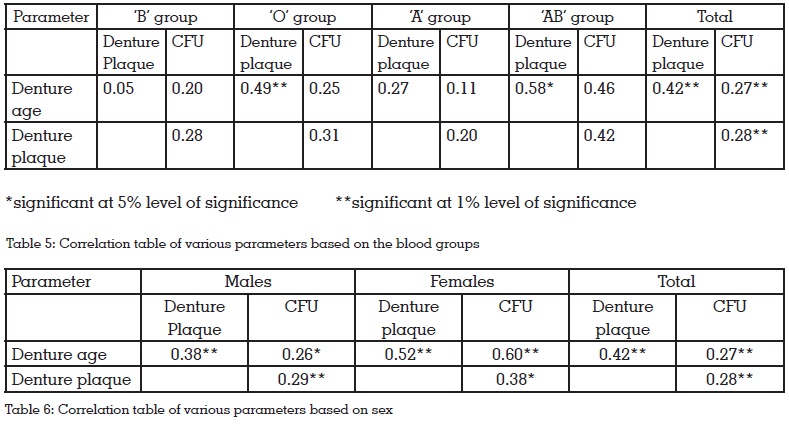
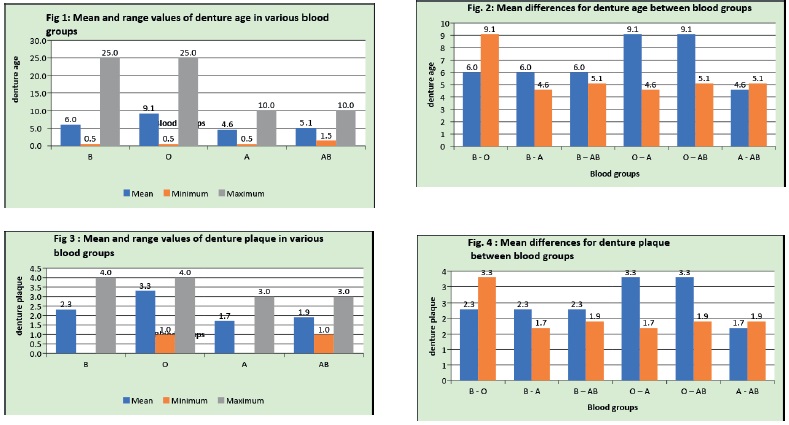
Table 2: demonstrates the age range (among
various blood groups) for which patients were
wearing dentures. Table 3: shows the degree of
denture plaque accumulation among various
blood groups. Table 5: demonstrates the degree
of oral Candidal colonization (CFU/ml) among
various blood groups. table 3: shows tendency
of blood group O to be a risk factor for increased
denture plaque accumulation. Therefore whether
the denture wearers in blood group O have a high
risk or not was examined using more sensitive statistical analysis. It was revealed that the amount
of denture plaque was significantly higher in
blood group O than in those subjects having other
blood types (p<0.05; Table 4) Furthermore, the
population with marked plaque accumulation
(grade 3, grade 4) was significantly higher in blood
group O than in those with other blood groups
(p<0.05; table 4) Discussion: Each individual has
a number of microorganisms in their oral cavity
but this microbial flora changes with respect to
presence or absence of teeth.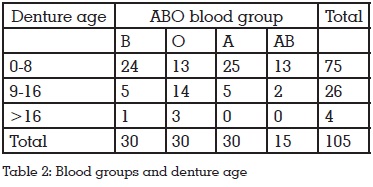
Candida species are the most common components
of human oral flora. Oral candidiasis (Candidal
count/ C.F.U is more than 200 cells/ml) is present
clinically in many forms reflecting its ability to
colonize different oral surfaces. Variety of systemic
and local factors predisposes the host to increased
Candidal colonization and subsequent infection.
It has been shown that the presence of dentures is
a predisposing factor to the onset of pathologies related to Candida. Clinical studies have shown
that C. albicans is not only able to adhere to the
mucosal surfaces, but also stick to the acrylic
resins of the dental prosthesis.6 Since one of the
major etiological factors of increased Candidal
carriage among denture wearers is considered to
be denture plaque accumulation on the denture
surface, Candida adherence to inert surfaces or
host cell surfaces is recognised as an initial step
in successful colonization and development of
pathogenesis.
The major human blood group system is ABO.
The blood group of a person depends upon the
presence or absence of two genes, A and B. the
majority of ABO determinants are expressed on the
ends of long polylactosamine chains. No diseases
are known to result from the lack of expression of
ABO blood group antigens, but the susceptibility
to a number of diseases has been interrelated
to a person’s ABO phenotype. Such correlations
remain conflicting and include the observation
that gastric cancer is common in blood group A
individuals, whereas gastric and duodenal ulcers
occur more commonly in group O individuals.
In India, data was lacking on association between
blood groups and degree of plaque accumulation
among denture wearers and our study aimed at
determining the same. The ultimate goal is to determine the blood group that is more susceptible
to oral Candidal carriage among denture wearers.
For the study, individuals were selected at random
form the O.P.D of the department of Prosthodontics,
of the institute. Patient’s consent was taken prior
to the onset of the study. Individuals requiring
complete dentures with at least six months of
denture wearing history comprise the study group
(n=105). While, the individuals with no denture
wearing history comprise the control group
(n=105). Blood samples of each individual were
collected to determine the blood type (Department
of Oral and maxillofacial pathology). The samples
were again subdivided according to their blood
types (A/B/AB/O).
Information was obtained through the structured
interview regarding personal details, chief
complaint, past and present medical history.
Individuals were asked about denture wearing
history (denture age), denture hygiene and denture
wearing habits. Assessment of the denture hygiene
was done by the prosthesis hygiene index as
described by Tarbet.
After obtaining the complete data, it was
statistically analysed and significance was set
at (p<0.05).
Significant differences were observed in the degree
of denture plaque accumulation among blood
groups A, B, AB and O. Blood group O shows higher
degree of denture plaque accumulation (grade
3, grade 4) as compared to other blood groups.
Nikawa et al (1992) conducted a similar study to
investigate the association between degrees of
denture plaque accumulation and ABO blood
types in denture wearers. They too concluded that
blood group O is a risk factor for denture plaque
accumulation.
The reason for this may be due to the fact that
the adherence of Candida to bare acrylic resin
surfaces or to solid surfaces is considered to be
mediated mainly by non-specific interaction. The
salivary proteins adsorbed to inert surfaces affect
the adherence of Candida, and it is suggested
that these proteins provide specific receptor
sites. Also the in-vivo adherence of Candida to denture surfaces might be affected by body fluids
containing immunodominant glycocompounds of
some blood types.
In our study, we found that as the degree of denture
plaque accumulation is increased, degree of oral
Candidal colonization is also increased. This
suggests that denture plaque accumulation might
be a risk factor for increased Candidal carriage.
The amount of denture plaque accumulation
was significantly higher in blood group O than
in other types (p<0.05) Thus, populations with
marked plaque accumulation (Grade 3, 4) were
significantly higher in blood group O than in those
with other blood types.
Elderly individuals show a
predisposition towards disease of oral cavity
where the high frequency of Candidal carriage
in the elderly suggests that with age the oral
environment becomes permissive to Candida.
This Candidal colonization in elderly is further
enhanced by the use of dentures. Through many
years researchers worked on several aspects of presence of Candida in elderly. This study was
intended to determine the relationship between
degree of denture plaque accumulation and ABO
blood types among denture wearers. The study
consisted of 210 patients, which were divided
in to study group (group A) and control group
(group B). The groups were further divided into
four subgroups according to ABO blood group
system. Blood group A consists of 60 patients (30
study and 30 control), Blood group B consist of 60
patients (30 study and 30 control), Blood group O
consist of 60 patients (30 study and 30 control), and
since Blood group AB is most rarely found, sample
size was limited to 30 (15 study and 15 control).
Denture hygiene was accessed by Tarbet’s denture
hygiene index and Blood groups were determined
by direct Heamagglutination method. Then the
data was statistically analyzed using chi square,
student t-test, one way ANOVA and tukey HSD.
Our study demonstrated that the denture plaque
was significantly increased in blood group O. Our
study thus stated that the blood group O is more
susceptible to denture plaque accumulation. The reason behind this increased susceptibility might
be due to the fact that the blood group O does not
have any antibody on their blood cell surface which
plays an important role against the attachment of
Candidal species to the host cell surface or inert
surface invivo.
The pathogenesis of Candida infections is
complex and involves both yeast and host related
factors. This aspect of host-fungal relationship is
illustrated by the spectrum of clinical presentation
of oral candidiasis. The repertoire of adherence
mechanisms exhibited by Candida albicans
enables it to colonize many oral niches. The ability
of Candida strain to overcome the host clearance
mechanisms and to colonize surfaces depends
on the effectiveness of those mechanisms, yeast
adherence, and the yeast growth rate. Progress
from the adherent replicating yeast to a mucosal
infection again depends upon adherence and
growth rate but also involves tissue penetration. For
an infection to persist, the host immune system must
fail to contain the growth of the yeast. The balance
among clearance, colonization, or candidiasis
therefore depends upon the ability of the Candida
strains to modulate expression of virulence factors
in response to environmental change, combined
with competence of host immune system. The
precarious nature of this balance is evidenced
by the significant number of people for whom
oral candidiasis is recurrent problem. The key
role played by adherence mechanisms suggests
that further molecular analysis of C. albicans cell
surface macromolecule expression and related
functions will ultimately provide the information
needed for effective prevention of oral candidiasis.
Efficient cleaning of dentures should be carried
out as the fungal growth on denture surface infect
and re-infect the soft tissues. The therapeutic
strategy should include the use of topical
(loscetar, amorolfine) and systemic antifungal
drugs (nystatin, amphotericin B, miconazole and fluconazole) the use of preservatives and
disinfectants (dentures immersed in two%
chlorhexidine or in 0.02% sodium hypochlorite),
the irradiation with microwaves and scrupulous
removal and control of the plaque present on the
denture and on the oral mucosa.
Good oral hygiene can be alone effective in treating
Candida-associated denture stomatitis when used
in conjunction with systemic and topical antifungal
agents. The hygiene control of denture is also
essential to avoid relapses of pathology following
treatment with antifungal drugs, and therefore,
it is an important measure for the prophylaxis of
oral candidiasis. Both the prosthesis and the oral
mucosa in contact with it must be involved in the
procedures for oral hygiene through brushing
them after each meal with or without chemicals.
The patient should be instructed to remove the
denture during night and to leave it dry. In addition,
during therapy, the prosthesis should be removed
for atleast two weeks.
Metal base maxillary dentures and high impact
acrylic resin have shown less penetration and
adherence of Candidal cells as compared to
conventional and tooth coloured acrylic, thus, the
use of these denture base materials might be of
clinical significance as a treatment alternative to
patients who are more prone to higher incidence
of fungal infections. Routine follow-up visits to a
dentist should be performed to assess that the
prosthesis maintains proper fit and function,
and that users are maintaining denture hygiene
instructions.
Oral health awareness and education programmes
should be conducted at the community level for
older population. The role and proper method of
oral hygiene practice, care for artificial dentures,
and self assessment of the oral cavity for early
detection of diseased condition should be explained
to the patient. In an effort to empower the elderly
in self-help and care, the educational material in different local languages should be produced
and distributed freely. Lastly, as a preventive
measure, education should be imparted to the
young population so that they retain their teeth in
optimal health and prevalence of dental disease
will be reduced. Research should be pursued in
various aspects of ageing and age related oral
health problems, including epidemiological studies
to measure the burden of oral diseases, the impact
of oral diseases on nutrition and general health,
the impact of interventions and so forth.